New Biomarker: iAP Accurately Diagnoses Deadly Infant Disease Called NEC (Necrotizing Enterocolitis).
Source: Thailand Medical News Nov 09, 2019 6 years, 3 months, 2 weeks, 4 days, 3 hours, 36 minutes ago
Researchers and clinicians at LSU Health New Orleans School of Medicine have discovered a new biomarker, a protein called
iAP for the noninvasive detection of
necrotizing enterocolitis (
NEC) that only mostly affects infants. The diagnostic study was one of the largest prospective clinical studies in premature infants yet, involved 136 premature infants.
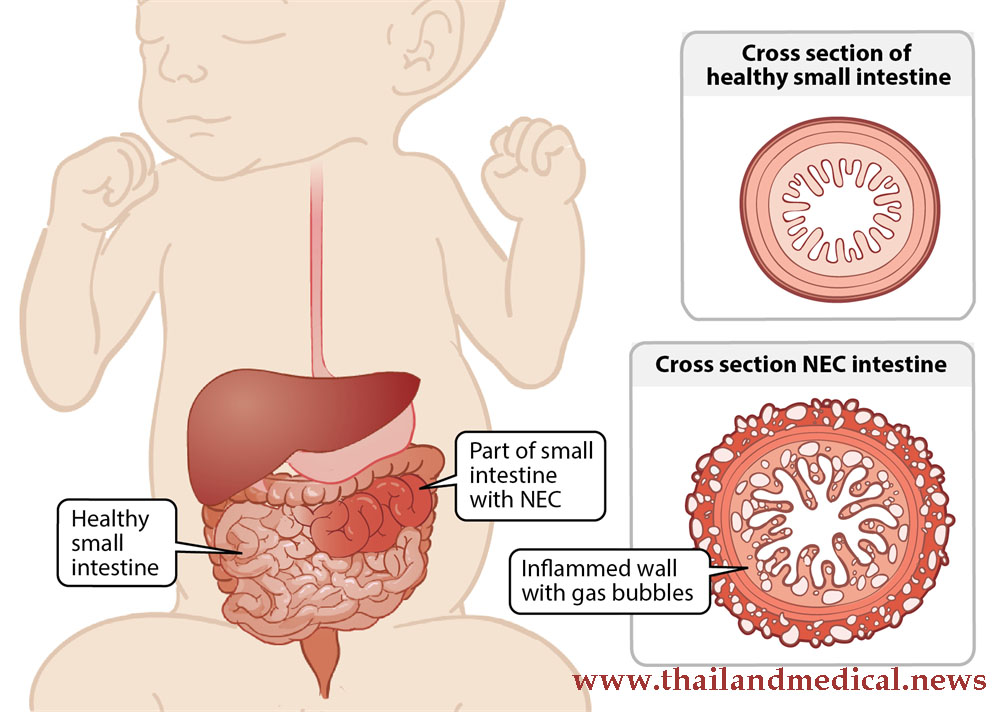
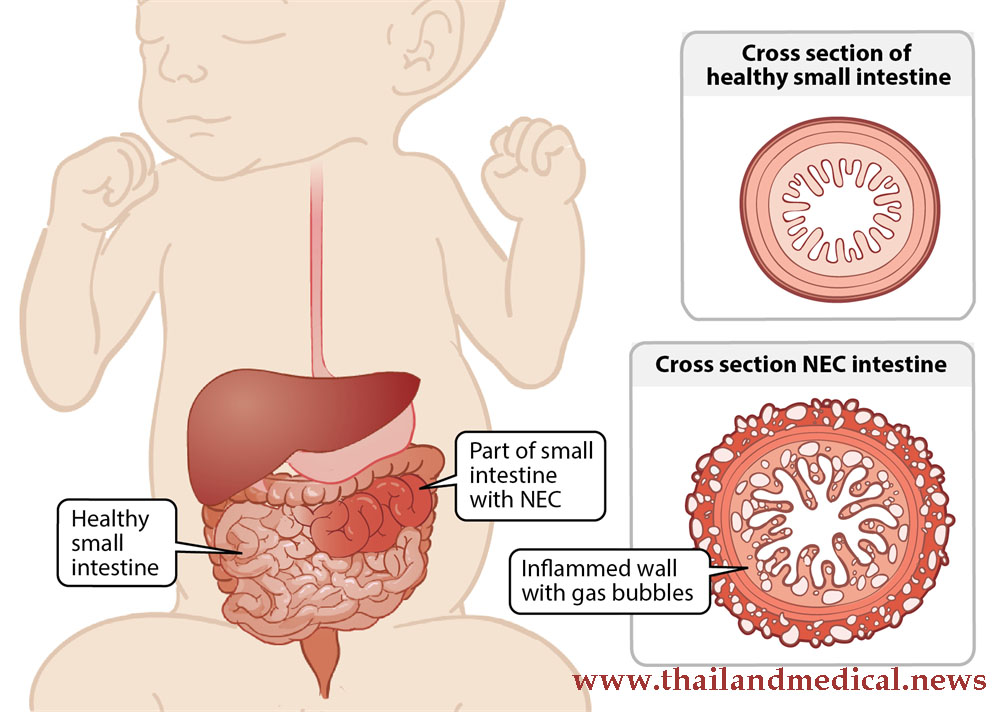 Necrotizing enterocolitis
Necrotizing enterocolitis is a life-threatening illness almost exclusively affecting neonates.
NEC has a mortality rate as high as 50%. Inflammation of the intestine leads to bacterial invasion causing cellular damage and cell death, which causes necrosis of the colon and intestine. As
NEC progresses, it can lead to intestinal perforation causing peritonitis, sepsis and death. To date, no clinical test has been established as the gold standard to diagnose NEC. X-rays are used to diagnose advanced disease, but their sensitivity can be as low as 44%.
Dr Sunyoung Kim, Ph.D., Professor of Biochemistry and Molecular Biology at LSU Health New Orleans School of Medicine and senior author told
Thailand Medical News, "This study exemplified academic medicine at its best. It creates linkages between unexplained patient presentations and scientific inquiry. We were driven by the desire to build unique and useable tools to fight a disease that has been unexplained for nearly 200 years in the most fragile patient population, preemie babies."
Past research suggested that
NEC is preceded and accompanied by changes in the complex and dynamic collection of microorganisms called gut microbiota, which live in the intestine. In this study, the research team measured and analyzed the activity of the protein, intestinal alkaline phosphatase (
iAP) obtained from stool samples from the babies enrolled in the study at Children's Hospital of New Orleans, Touro Infirmary, and St. Louis Children's Hospital. Clinical data collected included gestational age, birth weight, Apgar scores, delivery type, race, gender, feeding, antibiotics, laboratory and radiology results, as well as surgical notes. Eighteen percent of the babies were classified as having severe
NEC; 14% had suspected
NEC; and 68% were
NEC control.
Because
iAP activity precedes the chemical process triggering inflammation, the researchers studied the abundance and enzyme activity of
iAP shed in stool to assess the correlation of two
iAP biochemical measures with disease severity. They found that elevated levels of
iAP protein linked to
NEC were shed in the samples, but the proteins were dysfunctional in the NEC patients. The accuracy rates using
iAP levels and
iAP activity as markers for severe
NEC were 97% and 76%, respectively. The accuracy values were similar for suspected
NEC ,97% and 62%, respectively.
These findings indicate that
iAP biochemistry and abundance can be used as diagnostic biomarkers for both severe and suspected
NEC
strong>. Significantly, iAP measures were not biomarkers for sepsis, another potentially fatal condition that can exhibit symptoms similar to NEC. A correct diagnosis is crucial to treatment decisions.
The new biomarker has doubled the diagnostic identification of the disease, compared to the current gold standard a milestone important at both the bench and the bedside.
Dr. Kim further added "Intestinal AP is the first candidate diagnostic biomarker, unique in its predictive value for NEC. It is correlated only with NEC and is not associated with sepsis or other non-GI infections. The clinical potential of this noninvasive tool lies in its use to identify infants most at risk to develop NEC, to facilitate management of feeding and antibiotic regimens, and monitor response to treatment.”
The team is planning more clinical studies before submitting it to regulatory bodies and medical councils to adopt the new biomarker as a to be adopted standard diagnostic platform for NEC in infants.
Reference: JAMA Network Open (2019). DOI: 10.1001/jamanetworkopen.2019.14996