Emerging Studies Showing Role Of Gut Microbiome In COVID-19 And Benefits Of Probiotics For Treatments And As Prophylactics
Source: Probiotics-COVID-19 Nov 06, 2020 5 years, 3 months, 4 days, 3 hours, 39 minutes ago
Probiotics-COVID-19: Researchers from Department of Food and Nutritional Sciences, University of Reading-UK and Department of Sport Science, Sport, Health and Performance Enhancement Research Centre, Nottingham Trent University-UK have in a new study demonstrated the role of the gut microbiome in COVID-19 and also the benefits of probiotics for both as adjuvants and also as prophylactics.
The ongoing SARS-CoV-2 pandemic has altering the face of science and medicine, social interaction and public health worldwide. It has had a destructive effect upon millions of people and is approaching a devastating 1.3 million fatalities. New emerging evidence has suggested a link between the infection and gut microbiome status. This is one of several factors that may contribute towards severity of infection. Given the fact that the gut is heavily linked to immunity, inflammatory status and the ability to challenge pathogens, it is worthwhile to consider dietary intervention of the gut microbiota as means of potentially challenging the viral outcome. In this context, probiotics and prebiotics have been used to mitigate similar respiratory infections.
In this study the researchers summarize links between the gut microbiome and COVID-19 infection, as well as propose mechanisms whereby probiotic and prebiotic interventions may act.
The study findings were published in the British Journal Of Nutrition.
https://www.cambridge.org/core/journals/british-journal-of-nutrition/article/mechanisms-linking-the-human-gut-microbiome-to-prophylactic-and-treatment-strategies-for-covid19/A3E1ADF2053768F34BCA72BF620AC86F
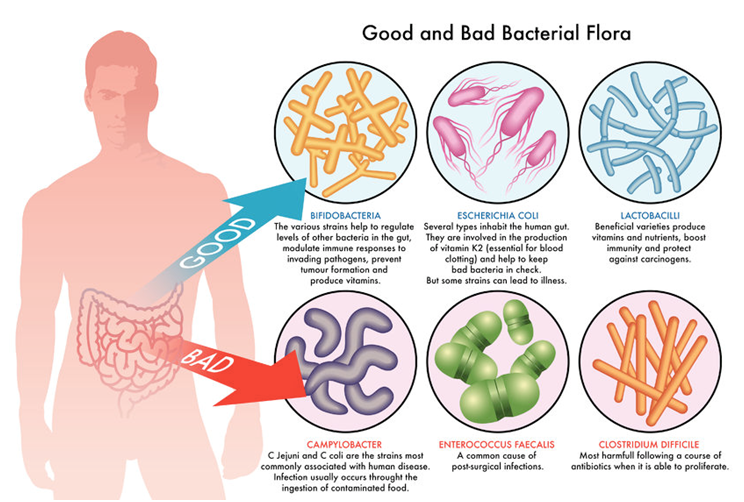
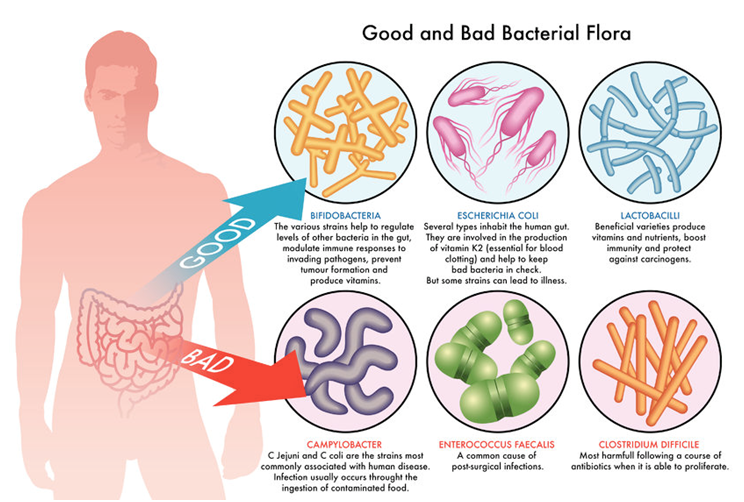
According to the research team, the different components of large intestinal microbiota may be considered as exerting potentially health-promoting or pathogenic effects. In the gut, resilience is connected to the functional core microbiota.
https://www.pnas.org/content/108/Supplement_1/4554
There are several mechanisms whereby the gut microbiota may influence viral transmission and disease progression. In relation to initial infection, a past study compared the faecal microbiota of 15 COVID-19 patients to healthy controls.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7237927/
When focusing on the microbiota of the 7 antibiotic naïve COVID-19 patients on admission to hospital, microbial sequencing revealed elevated levels of Coprobacillus spp. Clostridium ramosum and Clostridium hatherwayi were associated with severity of COVID-19 symptoms along with reduced levels of Alistipes spp. and the anti-inflammatory associated Faecalibacterium prausnitzii.
Coprobacillus spp. have been observed to upregulate ACE2 in the murine gut thus, changes in the gut microbiota may alter ability of the virus to gain cellular entry into the gut.
https://pubmed.ncbi.nlm.nih.gov/28215708/
Also it was found that immune changes brought about by the gut mi
crobiota can influence respiratory conditions.
https://www.frontiersin.org/articles/10.3389/fcimb.2020.00009/full
Past scientific evidence from studies has indicated that inhabiting gut microbiota shapes anti-viral defenses and could modulate outcomes in certain viral infections.
https://pubmed.ncbi.nlm.nih.gov/22168422/
The effects of differences in the gut microbial community have been demonstrated in viral infections like influenza and pneumonia. Numerous studies have even focused on modulation of gut microbial patterns and its effect on upper respiratory tract infections (URTI); bringing out through three meta-analyses reporting that probiotics can reduce severity and duration of illness.
https://pubmed.ncbi.nlm.nih.gov/24780623/
COVID-19 most commonly presents as a URTI but can, in a more severe spectrum, may attack the lungs to become a threatening lower respiratory tract infection (LRTI). Whilst evidence is constantly in progress, recent meta-analyses of randomized control trials have indicated that probiotics can reduce the incidence and severity of ventilator-associated pneumonia.
https://pubmed.ncbi.nlm.nih.gov/32127415/
Another recent study also showed supplementation with probiotics shortened the duration of ventilator use in critically ill patients. Similar findings have been observed in other ventilator-associated pneumonia studies, indicating that modulation of gut microbiota may also have a part to play in LRTI.
https://pubmed.ncbi.nlm.nih.gov/30088841/
Importantly there is a durable amount of evidence supporting a prophylactic role of probiotics in reducing symptoms associated with upper respiratory tract infections. Studies modelling the impact of probiotic consumption on respiratory infections in the pre-COVID-19 era have emphasized economic savings with the use of probiotic consumption in the general population.
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0166232
Research has shown that by supplementation with probiotics, which means adopting a strategy towards correcting gut dysbiosis and increasing levels of positive microorganisms in the gut can impact multiple pathways that could be of benefit in the fight against COVID-19, summarized as given below:
1) Supplementation with probiotics positively modulates the bacterial community in the gut, often to the detriment of potentially pathogenic microorganisms, through the production of metabolites and/or competitive exclusion. This can reduce the risk of gut- related illnesses.
2) It is known that the gut microbiota secretes short-chain fatty acids (SCFA) that may have systemic effects across the body, including the provision of a cellular energy source.
3) Importantly increased SCFA levels are associated with improved integrity of tight intestinal junctions, possibly restricting the passage of endotoxin from the gut lumen; such effects may be partly mediated by cytokines. It is noteworthy that both aging and obesity which are risk factors for COVID-19, are associated with a more vulnerable gut barrier function.
4) Free fatty acid receptors can be found on dendritic cells, as such SCFA stimulation of dendrites can lead to interaction with regulatory T-cells, subsequently resulting in enhanced macrophage activity and increased anti-inflammatory cytokines.
5) Macrophages are associated with pro-inflammatory status, and SCFA has been observed to down-regulate pro-inflammatory cytokine release.
Hence by supporting the immune responses and reducing aggressive inflammatory activity, harmonizing the gut microbiota through the use of probiotics could be a tool to aid the body in defending against COVID-19
A recent interesting study examined seventy COVID-19 positive patients requiring non-invasive oxygen therapy who were treated with hydroxychloroquine therapy along with antibiotics and tocilizumab; and in it, a subgroup of 28 of these, an oral probiotic mixture was also administered.
https://www.frontiersin.org/articles/10.3389/fmed.2020.00389/full
Significantly, along with clinical improvement reported in digestive symptoms, the probiotic group had an eight- fold reduction in the risk of developing respiratory failure.
Study results like these bring out great potential for considering to use probiotics to combat respiratory difficulties. As clinical evidence continues to develop in this direction, the role of safe and cost-effective probiotic interventions against COVID-19 infection could become more important.
Another interesting point is that it has been reported that variations in the intestinal microbiome may compromise the effectiveness of vaccine antigens, a result of chronic inflammation of the intestinal tract. Falling along the same lines, a meta-analysis of probiotic studies has concluded that intervention alongside influenza vaccination can lead to elevated immunogenicity through enhancing seroconversion of inoculated persons. Such data suggest interesting clinical implications for the population in the near future while the discovery of the COVID-19 vaccine is underway
https://pubmed.ncbi.nlm.nih.gov/29232932/
https://pubmed.ncbi.nlm.nih.gov/29909134/
There is currently clinical evidence progressing along the direction that modulation of gut microbiota, resolving the gut dysbiosis can positively influence COVID-19 outcomes. This is further substantiated by the positive effects of probiotics reported against other coronavirus strains.
https://pubmed.ncbi.nlm.nih.gov/23188495/
While studies are underway globally to assess whether altering the gut microbiota through diet and supplementation might be a feasible addition to our current COVID-19 treatment armamentarium; given the large experience of clinical usage, and evidence for beneficial effects in various clinical settings, Lactobacillus and Bifidobacterium can be safely considered.
https://pubmed.ncbi.nlm.nih.gov/32921328/
In China, recommendations have been made with regards to modifying the gut microbiota to improve outcomes in patients with severe COVID-19 symptoms.
https://en.nhc.gov.cn/publications.html
These recommendations were based on observed differences in the faecal microbiota in those with COVID-19 compared to healthy controls which suggested that the virus can replicate and exist in the digestive tract(98) .
https://regional.chinadaily.com.cn/pdf/DiagnosisandTreatmentProtocolforCOVID-19Patients(Tentative8thEdition).pdf
A Chinese study reported the presence of gastrointestinal symptoms in half of COVID-19 patients within a group of hospitalized Chinese patients with disease severity correlating with the severity of gut symptoms. This a clear demonstration that, in China at least, the gut microbiota is considered to be an important influencer on COVID-19 outcome.
https://pubmed.ncbi.nlm.nih.gov/32287140/
There is currently clinical evidence gathering to indicate that modulation of the gut microbiota can positively influence COVID-19 disease progression. This is further supported by reported positive effects of probiotics against other coronavirus strains.
https://link.springer.com/article/10.1007/s00705-012-1543-0
Detailed studies are underway across the globe to investigate whether altering the gut microbiota through diet might be a feasible addition to our COVID-19 treatment armoury and recently, one study have suggested specific evidence-based probiotic products that may have relevance to reducing the coronavirus pandemic burden.
https://www.frontiersin.org/articles/10.3389/fpubh.2020.00186/full
The race for a vaccine and pharmaceutical treatments for the current COVID-19 pandemic continues. However, both are likely to be some way from routine use and, in the meantime, attention should be given to emerging, but convincing, evidence that gut health may be related to COVID-19.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7162053/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7217790/
https://ccforum.biomedcentral.com/articles/10.1186/s13054-020-03043-w
The approaches suggested here to improve gut microbial health are safe and straightforward to implement and have a scientific basis. In the current climate, a reduction in illness severity and duration could be an asset not only to health systems worldwide, but also to those suffering with COVID-19.
There are also numerous other studies supporting the usage of probiotics for COVID-19.
https://www.nature.com/articles/s41538-020-00078-9
https://www.tandfonline.com/doi/full/10.1080/09637486.2020.1807475
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7434852/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7357989/
https://www.thelancet.com/pdfs/journals/langas/PIIS2468-1253(20)30195-3.pdf
https://www.cambridge.org/core/journals/british-journal-of-nutrition/article/probiotics-and-covid19-think-about-the-link/AA1BA92236F8A63EF39FFC166562E435
For more on
Probiotics-COVID-19, keep on logging to Thailand Medical News.