Vitamin A Plays A Key Role In Enhancing Mucosal Immunity Against Omicron COVID-19 Infections
Nikhil Prasad Fact checked by:Thailand Medical News Team Mar 09, 2024 1 year, 11 months, 1 week, 12 hours, 1 minute ago
COVID-19 News: Respiratory tract infections (RTIs) continue to be a global health challenge, with lower RTIs ranking as the fourth leading cause of mortality worldwide. The persistent threat of the COVID-19 pandemic, compounded by the emergence of the Omicron variant, underscores the critical need for effective immune responses to combat evolving viral strains. Mucosal immunity, particularly the production of secretory immunoglobulin A (SIgA), has emerged as a key player in defending against respiratory infections. This
COVID-19 News report delves into a cross-sectional study conducted by researchers from the Universidad de Guadalajara-Mexico and the University of Catania-Italy, aiming to unravel the intricate relationship between vitamin A status and SIgA levels in COVID-19 outpatients, specifically those infected with the Omicron variant.
 Vitamin A Plays A Key Role In Enhancing Mucosal Immunity Against Omicron COVID-19 Infections
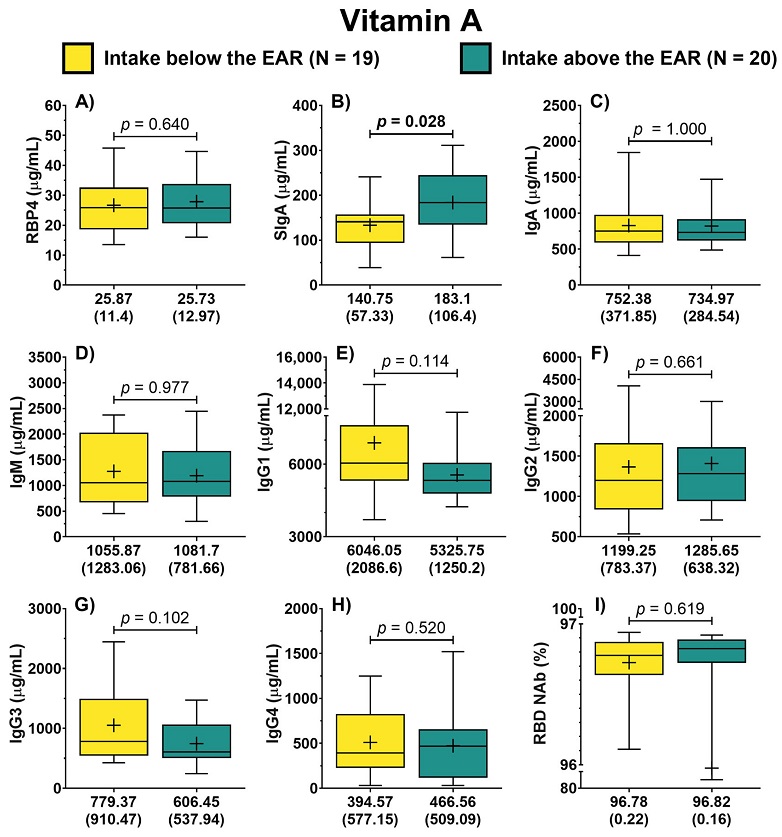
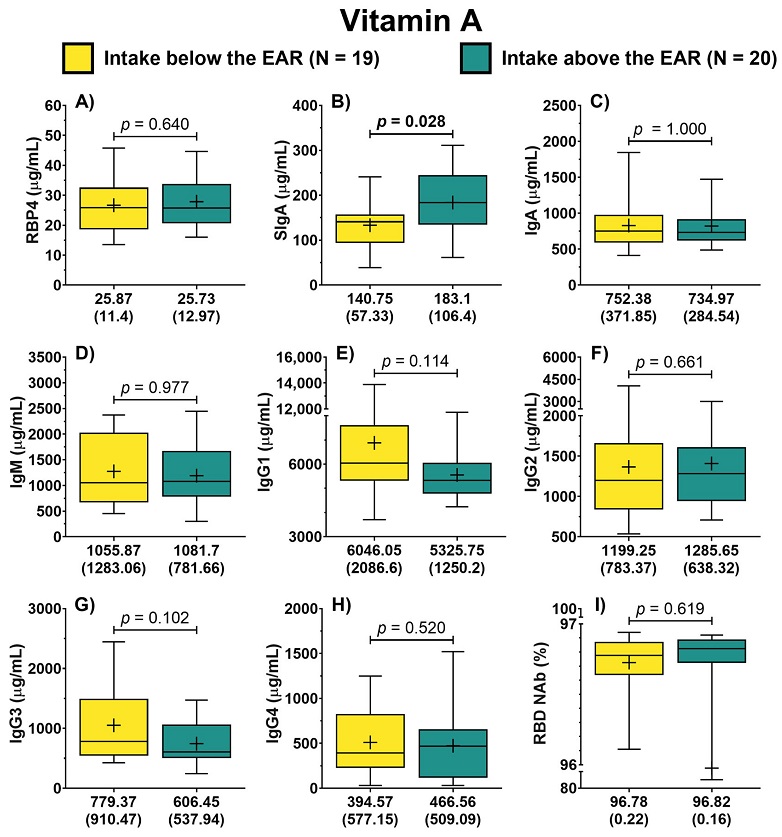
Antibody concentration according to the dietary intake of vitamin A of COVID-19 outpatients. RBP4 levels in patients with either dietary intake below or above the EAR (A). The levels of the different antibody isotypes and RBD NAb in patients according to the classification of vitamin A intake (B–I). The description for each graph includes the median with the interquartile range, Mann–Whitney U test. Bold formatting is used to highlight significant p-values. Abbreviations: EAR, estimated average requirement; RBP4, retinol-binding protein 4; Ig, immunoglobulin; RBD NAb, receptor-binding domain neutralizing antibodies; hs-CRP, high-sensitivity C-reactive protein; IL-6, interleukin 6; TGF-β1, transforming growth factor beta 1.
The Importance of Mucosal Immunity in Respiratory Infections
Vitamin A Plays A Key Role In Enhancing Mucosal Immunity Against Omicron COVID-19 Infections
Antibody concentration according to the dietary intake of vitamin A of COVID-19 outpatients. RBP4 levels in patients with either dietary intake below or above the EAR (A). The levels of the different antibody isotypes and RBD NAb in patients according to the classification of vitamin A intake (B–I). The description for each graph includes the median with the interquartile range, Mann–Whitney U test. Bold formatting is used to highlight significant p-values. Abbreviations: EAR, estimated average requirement; RBP4, retinol-binding protein 4; Ig, immunoglobulin; RBD NAb, receptor-binding domain neutralizing antibodies; hs-CRP, high-sensitivity C-reactive protein; IL-6, interleukin 6; TGF-β1, transforming growth factor beta 1.
The Importance of Mucosal Immunity in Respiratory Infections
The COVID-19 pandemic has highlighted the significance of mucosal immunity in protecting against infectious agents, particularly the SARS-CoV-2 virus responsible for COVID-19. The primary transmission route of SARS-CoV-2 emphasizes the crucial role of the immune response in the respiratory mucosa. Within this context, SIgA, a vital antibody produced in significant quantities in the mucosal surfaces, plays a pivotal role in the defense against respiratory infections. Targeting the production of SIgA has been proposed as an effective strategy for preventing respiratory infections, given its key role in neutralizing and preventing the entry of pathogens.
Vitamin A's Role in Mucosal Immunity
Vitamin A, a fat-soluble compound obtained through dietary intake, has long been recognized for its influence on the immune system. Its metabolism leads to the production of retinoic acid (RA), acting as a transcription factor that regulates various immune system functions. Vitamin A is particularly crucial for mucosal immunity, where RA contributes to the class switch to IgA in gut-associated lymphoid tissues (GALTs). The connection between vitamin A deficiency and respiratory infections has been expl
ored in preclinical studies, showing that deficient diets lead to lower SIgA concentrations. Conversely, studies in mice have demonstrated that a vitamin A-rich diet or vitamin A supplementation enhances SIgA concentrations in response to respiratory viruses.
Human Studies and the Correlation between Vitamin A and SIgA
While less explored, human serum samples have indicated positive correlations between retinol concentrations and the IgA/IgM ratio, serving as an indicator of class switch recombination. Additionally, correlations have been observed between retinol-binding protein 4 (RBP4), the main vitamin A transporter protein, and IgA concentrations. Against this backdrop, the present cross-sectional study aimed to investigate the relationship between vitamin A nutritional status and SIgA levels in COVID-19 outpatients infected with the Omicron variant.
Study Design and Participant Characteristics
The study included 39 COVID-19 outpatients diagnosed with the Omicron variant, evaluated 14 days post-diagnosis. Notably, all patients had experienced COVID-19 for the first time, with common persistent symptoms including phlegm, cough, headache, constipation, and weakness. The participants had received COVID-19 vaccinations, primarily Pfizer/BioNTech and CanSino. Serum analysis revealed concentrations of IL-6 and hs-CRP, providing insights into the inflammatory status.
Assessment of Vitamin A Nutritional Status
The nutritional status of vitamin A was evaluated based on dietary intake and the analysis of retinol-binding protein 4 (RBP4). Dietary intake revealed that nearly half of the patients did not meet the estimated average requirement (EAR) for vitamin A, and the majority did not reach the recommended dietary allowance (RDA). RBP4 concentrations, a key marker of vitamin A status, indicated insufficiency in over one-third of the patients.
Correlation of Antibodies with Vitamin A Nutritional Status
Analysis of serum antibodies revealed intriguing correlations with vitamin A nutritional status. Patients with higher vitamin A intake exhibited significantly higher SIgA concentrations, along with elevated SIgA/IgG1 and SIgA/IgG3 ratios. Similarly, patients with higher RBP4 levels showed increased SIgA/IgM, SIgA/IgG1, and SIgA/IgG2 ratios. These findings underscored a direct correlation between vitamin A nutritional status and SIgA levels in COVID-19 outpatients.
Detailed Correlation Analysis
Further correlation analysis delved into the relationships between dietary vitamin A intake, RBP4 levels, and various immune parameters. Positive correlations were identified between vitamin A intake and RBP4, as well as with SIgA. Conversely, a negative correlation was observed between vitamin A intake and IgG1 concentrations. RBP4 exhibited positive correlations with SIgA and negative correlations with multiple immunoglobulin classes, including IgA, IgM, IgG1, and IgG2. Additionally, the study explored the correlation of vitamin A intake and RBP4 with symptom scores, revealing trends toward a negative correlation.
Clinical Implications and Future Directions
The study's findings suggest a significant prevalence of suboptimal vitamin A intake and insufficient RBP4 concentrations in COVID-19 outpatients, despite previous vaccination. The correlation of these nutritional factors with enhanced SIgA levels implies a potential role for maintaining optimal vitamin A levels in preventing viral infections, particularly respiratory tract infections. Addressing vitamin A deficiency through dietary interventions or supplementation may serve as a prophylactic strategy against respiratory infections.
Conclusion
In conclusion, the intricate relationship between vitamin A status and SIgA response in COVID-19 outpatients infected with the Omicron variant highlights the potential significance of nutritional interventions in enhancing mucosal immunity. The positive correlations observed between vitamin A intake, RBP4 levels, and SIgA levels underscore the potential role of vitamin A in preventing the incidence and progression of respiratory infections. As the global community continues to navigate the challenges of the COVID-19 pandemic, understanding the interplay between nutrition and immune responses becomes increasingly crucial in developing effective preventive strategies.
The study findings were published in the peer reviewed Journal of Clinical Medicine.
https://www.mdpi.com/2077-0383/13/6/1538
For the latest
COVID-19 News, keep on logging to Thailand Medical News.