German scientists uncover how SARS-CoV-2's spike protein influences blood clotting and immune response
Nikhil Prasad Fact checked by:Thailand Medical News Team Sep 30, 2024 1 year, 4 months, 2 weeks, 6 hours, 5 minutes ago
Medical News: Researchers from the Charité Universitätsmedizin in Berlin and other collaborators have made significant discoveries regarding the interaction of SARS-CoV-2’s spike protein with a key blood protein, fibrinogen. This interaction sheds light on the clotting problems and immune responses observed in COVID-19 and post-COVID-19 conditions. The findings not only provide deeper insight into the underlying mechanisms but also suggest potential therapeutic approaches for COVID-19. This
Medical News report highlights the important discoveries made in their research.
 German scientists uncover how SARS-CoV-2's spike protein influences blood clotting and immune response
Spike Protein and Fibrinogen Interaction
German scientists uncover how SARS-CoV-2's spike protein influences blood clotting and immune response
Spike Protein and Fibrinogen Interaction
In a recent study led by Dr. Tom Aschman and Dr. Helena Radbruch, the team investigated the relationship between the SARS-CoV-2 spike protein and fibrinogen, a blood protein responsible for forming clots. Previous research had indicated that the spike protein could bind to fibrinogen, but the team wanted to explore this connection further.
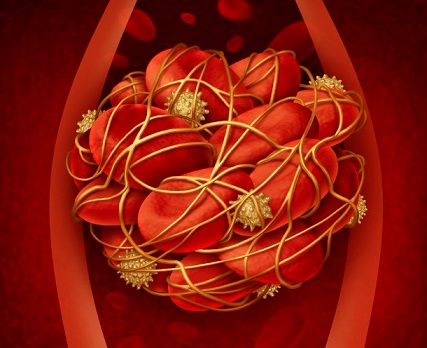
Using laboratory experiments with mice and human plasma, the team demonstrated that the spike protein binds to fibrinogen and its polymerized form, fibrin. The spike protein was found to affect blood clot formation by altering the structure of the clots and accelerating the clotting process when present with thrombin. Furthermore, the researchers discovered that the presence of the spike protein delayed the breakdown of clots, a process known as fibrinolysis. This interaction suggests why some COVID-19 patients experience severe clotting problems, which can lead to life-threatening conditions such as stroke, pulmonary embolism, and deep vein thrombosis.
Immune Response Alteration
In addition to the effects on clotting, the study revealed that the spike protein and fibrinogen interaction influenced the immune response, particularly the activity of natural killer (NK) cells. NK cells are crucial in fighting off viral infections, and their impaired function has been observed in severe cases of COVID-19. The researchers found that this impairment might be linked to the interaction between the spike protein and fibrin.
Mice that were genetically modified to lack fibrinogen or a specific binding site crucial for the spike protein-fibrinogen interaction exhibited reduced lung inflammation and damage after infection with SARS-CoV-2. These mice also showed fewer immune cells in the lungs, particularly macrophages and NK cells. The team hypothesized that the spike protein disrupts NK cell function by influencing fibrinogen’s role in immune responses, which could lead to a failure in clearing the virus effectively in some patients.
This altered immune response could also contribute to the prolonged symptoms seen in post-COVID-19 condition (PCC), commonly known as long COVID, where patients continue to experience health issues long after the virus has left their system.
Study Methodology and Fi
ndings
The study employed a combination of in vitro (laboratory-based) and in vivo (animal-based) experiments to analyze the spike protein’s role in coagulation and immune system response. In vitro experiments showed that when human plasma was incubated with the spike protein, the structure of blood clots was noticeably altered, and clot formation was faster. Scanning electron microscopy confirmed these findings, showing that the spike protein directly influences clot structure.
In vivo experiments were conducted on genetically modified mice. The mice were either deficient in fibrinogen or lacked a specific motif (γ390–396) involved in immune receptor activation. When these mice were infected with SARS-CoV-2, they exhibited reduced lung damage and inflammation compared to normal mice.
The genetically altered mice also showed lower levels of type I interferon responses, a marker of severe COVID-19. The results suggest that fibrinogen plays a critical role in both clotting and immune responses during COVID-19 infection, and its interaction with the spike protein exacerbates the severity of the disease.
Potential for New Treatments
One of the most promising aspects of this study is the potential for new therapeutic approaches to COVID-19. The researchers highlighted that an antibody known as 5B8, which blocks a specific region of fibrin, could reverse some of the negative effects caused by the spike protein. In their experiments, the administration of 5B8 reduced oxidative stress and macrophage activation in the lungs of infected mice, suggesting that this treatment could be beneficial in reducing inflammation and lung damage in COVID-19 patients.
While vaccines remain the most effective prophylactic measure against COVID-19, the researchers suggested that therapies targeting the spike protein-fibrinogen interaction could serve as additional treatment options, particularly for patients at risk of severe disease or those suffering from PCC. However, they also noted that more research is needed to determine the feasibility and safety of such treatments in humans.
Limitations of the Study
Despite the promising findings, the researchers emphasized that the study had several limitations. The experiments were conducted primarily in mice, and while they provide valuable insights into the mechanisms of COVID-19, further studies are needed to confirm whether the same processes occur in humans.
Additionally, the study focused on early infection stages, and the researchers did not assess long-term outcomes or survival rates in their mouse models. As such, it is unclear whether these findings would apply to later stages of the disease or the post-infectious phase.
Another important consideration is that the spike protein produced by COVID-19 vaccines does not appear to cause the same clotting problems in most recipients, indicating that the interaction between the spike protein and fibrinogen might be specific to the virus itself rather than the protein alone. Nevertheless, the study provides a crucial step toward understanding the complex interactions between SARS-CoV-2 and the human body, and it could lead to the development of new treatments for COVID-19 and PCC.
Conclusion
In conclusion, this study reveals how the SARS-CoV-2 spike protein’s interaction with fibrinogen contributes to clotting problems and immune system dysregulation in COVID-19. By binding to fibrinogen, the spike protein accelerates clot formation and hinders the natural breakdown of clots, which can lead to severe complications in patients. The spike protein also interferes with the function of NK cells, preventing the immune system from effectively clearing the virus.
The study suggests that therapies targeting the spike protein-fibrinogen interaction, such as the 5B8 antibody, could provide additional treatment options for severe cases or PCC. More research is needed to confirm these findings in humans and to explore the long-term effects of such treatments.
The study findings were published in the peer-reviewed journal: Trends in Immunology
https://www.cell.com/trends/immunology/fulltext/S1471-4906(24)00215-1
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/new-study-uncovers-key-role-of-micrornas-in-blood-clotting-during-severe-covid-19
https://www.thailandmedical.news/news/study-reveals-key-differences-in-blood-clotting-responses-between-covid-19-and-non-covid-sepsis-patients