Source: Gastric Reflux - COVID-19 May 01, 2022 3 years, 9 months, 1 week, 6 days, 34 minutes ago
Gastric Reflux - COVID-19: In the last 18 months, physicians and also entities involved with gastric reflux education and care for patients in the UK and the United States have been struck by the number of patients that who describe the sudden onset of reflux type symptoms.
Besides the typical heartburn esophageal type symptoms, other more commonly symptoms reported included laryngo-pharyngeal (LPR) problems including a sore throat, throat clearing, globus and dysphonia (husky voice).
Many times, the onset of these symptoms coincided with a positive PCR test and a diagnosis of COVID-19, sometimes with other symptoms which may or not have been a manifestation of COVID and sometimes in isolation, with patients otherwise remaining entirely well.
In one case report published in the American Journal of Gastroenterology, a patient developed symptoms of heartburn after anti-reflux surgery without evidence of surgical complications or improvement with medications. The timing of both exposure to SARS-CoV-2 and symptom onset was helpful in making a diagnosis of COVID-19 associated esophageal hypersensitivity.
https://journals.lww.com/ajg/fulltext/2020/10001/s2041_covid_19_associated_with_esophageal.2041.aspx
The incidence of gastric reflux though not common at that time, was already reported during the early days of the COVID-19 pandemic in China.
https://gut.bmj.com/content/69/6/997
Interesting, it is not suspected that some of the new emerging BA.2 subvariants like the BA.2.12 and more so the BA.2.3 and BA.2.3.4 subvariants are exhibiting a tropism towards the gastrointestinal tract and causing a variety of gut issues including acid reflux. In Alberta, Canada, where these variants are rampant, media reports are already showing an increase in gastrointestinal issues.
https://globalnews.ca/news/8800394/alberta-covid-19-gastro-symptoms/
Many doctors are also saying that gastric reflux is also a growing manifestation in Long COVID.
https://parade.com/1310612/emilyshiffer/is-heartburn-a-sign-of-covid/
A Harvard
Gastric Reflux - COVID-19 study has also confirmed that gastric reflux manifestations are a growing gastrointestinal issue in many Post-COVID-19 patients.
https://scholar.harvard.edu/cvt/covid-long-haulers-gastrointestinal-system%C2%A0
By now, everyone now knows that COVID-19 is a systemic disease and that its symptomatic presentation varies enormously. Every system in the body is at risk and neurological complications are now well recognized.
Studies have already shown the central nervous system involvement including encephalitis and encephalomyelitis as well as conditions caused by peripheral nerve injury such as Guillain-Barré syndrome.
A study from Wuhan reported that
in hospitalized patients up to a third presented with neurological complications. But as the pandemic progressed in 2020 clinicians and patients became aware that some of the more common symptoms included loss of smell and taste.
An epidemiological meta-analysis suggests that loss of smell (hyposmia) and loss of taste (hypogeusia) can occur in up to 20% of COVID patients.
It should be noted that taste is mediated by three of the twelve cranial nerves, the facial nerve (cranial nerve VII), which provides fibres to the anterior two-thirds of the tongue, the glossopharyngeal nerve (cranial nerve IX), which provides fibres to the posterior third of the tongue, and the vagus nerve (cranial nerve X), which provides fibres to the epiglottis region. Smell is mediated by the olfactory nerve (I).
Importantly there are also reports of involvement of other cranial nerves involvement in COVID patients, detected by clinical examination and/or magnetic resonance imaging (MRI) including facial paralysis and Bell’s palsy (VII), abducens nerve palsy (VI), and optic nerve (II) sheath enhancement.
However, the mechanism by which SARS-CoV-2 causes these manifestations remains unclear. It’s been suggested that the smell and taste problems may be related to direct infection of the nasal and pharyngeal mucosa including the so-called “olfactory cleft syndrome” in which a conductive loss is caused by mucosal obstruction of the olfactory cleft. Certainly, much of the systemic damage caused by COVID is secondary to well documented inflammatory mediated responses and other systemic mechanisms may include hypoxia and coagulopathy. However, it seems that there is some evidence that the virus might enter the central nervous system or peripheral nerves directly and indeed the olfactory bulb is a well described pathway for viral entry into the central nervous system.
The SARS-CoV-2 virus directly targets angiotensin converting enzyme 2 (AGE2) via its spike protein and their proteases are expressed in the olfactory epithelium. The COVID virus can cross through the respiratory epithelial barrier into the blood and lymphatic system and then the blood brain barrier into the central nervous system. ACE2 receptors are also expressed in the nervous system and viral RNA has been identified in the cerebro-spinal fluid of some affected patients and there are also case studies reporting brain abnormalities on MRI suggestive of direct viral involvement.
Hence, while the mechanism remains unclear there’s no doubt that COVID can cause symptoms associated with cranial nerve dysfunction.
Many of you would by now be asking how does all these relate to reflux?
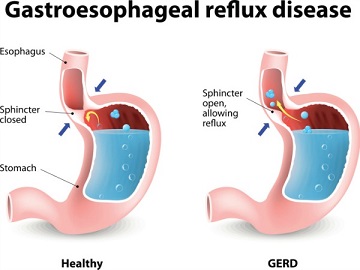
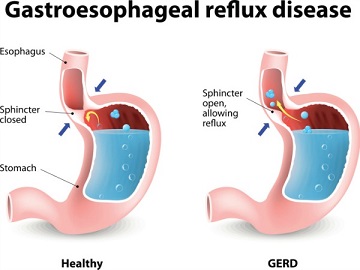
To begin with, the functions of the upper and lower esophageal sphincter mechanisms which protect the airway from gastro-esophageal reflux are mediated by multiple complex neurological reflexes. These involve the vagus and glossopharyngeal cranial nerves as well as the phrenic nerve which supplies the diaphragm.
There are already reports of phrenic nerve palsy in patients with COVID.
Thus, it seems quite reasonable to postulate that these reflexes may be disrupted by viral injury either directly or indirectly to one or perhaps several of the nerves involved in these neurological reflexes and that this then causes gastro-esophageal reflux.
Some doctors have witnessed many patients in whom their reflux symptoms have slowly resolved, which of course would be unusual in primary gastro-esophageal disease but consistent with transient neural injury as well as the usual slow resolution of taste and smell dysfunction following SARS-CoV-2 infections.
Importantly, there are other potential mechanisms that should be considered.
It has been found that alterations in the gut microbiome can cause reflux type symptoms.
A study published last year found that 60% of patients presenting for anti-reflux surgery have Small Intestinal Bacterial Overgrowth (SIBO). This condition is associated with the use of PPIs and anti-biotics as well as disrupted gastrointestinal motility.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8599257/
Whether COVID causes intestinal neurological injury is unknown but certainly gastrointestinal symptoms are well described in COVID and the gut is rich in angiotensin receptors. Fermentation by micro-organisms of sugars within the small bowel, which is usually relatively sterile, causes release of intra-luminal gas and consequent excessive belching. This belching of aerosolized gastric contents into the esophagus and throat is thought to cause reflux symptoms.
Already many studies have shown that SARS-CoV-2 causes gut microbiome dysbiosis.
https://www.frontiersin.org/articles/10.3389/fmed.2022.821777/full
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8198029/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8402052/
https://www.sciencedirect.com/science/article/pii/S0753332220311392
https://gut.bmj.com/content/71/3/544
https://www.biorxiv.org/content/10.1101/2021.07.15.452246v1
https://www.biocodexmicrobiotainstitute.com/en/pro/gut-dysbiosis-sars-cov-2-infected-monkeys
Such gut microbiome dysbiosis can also trigger gastric reflux.
It should be noted that, while offered as purely anecdotal evidence, many of the patients seen had been prescribed antibiotics to treat various manifestations of COVID and even more high doses of PPIs while GP services were being delivered remotely. Most of these patients, reported these as mostly ineffective.
Physicians diagnosed many of these patients with SIBO using lactulose hydrogen breath tests and their symptoms have often resolved following eradication.
A tantalizing question therefore is could a proportion of these patients’ symptoms all be secondary to SIBO?
Many of these questions remain unanswered and it’s likely that there are multiple mechanisms causing reflux symptoms.
Physicians however are convinced that whether directly or indirectly, COVID has been associated with reflux symptoms in some of the patients that they have seen over the past months.
More detailed research is warranted to provide the answers, especially to understand the mechanisms of how COVID affects the nervous system and cranial nerves in general, and the neural reflexes that normally prevent gastro-esophageal reflux in particular.
Physicians in the meanwhile are advising that patients with reflux symptoms be assessed against their whole symptom profile including those potentially caused by COVID and SIBO and that the prolonged use of PPIs that aren’t providing symptomatic relief should be avoided.
For more on
Gastric Reflux and COVID-19, keep on logging to Thailand Medical News.