French doctors warn that even mild COVID-19 can cause acute Cerebellitis that is difficult to diagnose
Nikhil Prasad Fact checked by:Thailand Medical News Team Sep 28, 2024 1 year, 4 months, 2 weeks, 2 days, 10 hours, 21 minutes ago
Medical News: An alarming clinical case study challenges medical expectations with normal test results.
A team of doctors in France recently reported a rare and life-threatening condition following a COVID-19 infection. A 32-year-old man, previously healthy, suddenly developed acute cerebellitis, a critical condition affecting the brain, after recovering from a mild COVID-19 infection. The case is notable because despite severe symptoms, laboratory tests and imaging results came back normal, confusing the doctors initially. This Medical News report explores this unusual case and sheds light on the importance of early treatment for cerebellitis even when diagnostic tests appear unremarkable.
 French doctors warn that even mild COVID-19 can cause acute Cerebellitis that is difficult to diagnose
Thailand Medical News
French doctors warn that even mild COVID-19 can cause acute Cerebellitis that is difficult to diagnose
Thailand Medical News had previously covered a study by Iranian doctors that found that COVID-19 can cause cerebellitis especially in males.
https://www.thailandmedical.news/news/covid-19-can-cause-cerebellitis-especially-in-males
This new study study was conducted by researchers from Nord Franche-Comté Hospital, France, led by Dr. Timothée Klopfenstein from the Department of Infectious and Tropical Diseases, along with a team of specialists including Samantha Poloni, Abdoulaye Hamani, Valentine Kassis, Pauline Escoffier, Beate Hagenkotter, and Souheil Zayet. Their detailed findings illustrate the complexity of COVID-19’s neurological impacts.
The Patient’s Sudden Deterioration
On October 31, 2023, a previously healthy 32-year-old man was rushed to the emergency room. He presented with troubling neurological symptoms, including difficulty speaking (dysarthria) and problems walking, combined with a high fever of 38.7°C. Interestingly, the patient did not show signs of seizures, altered consciousness, or coma. His neurological symptoms began just two weeks after recovering from a mild respiratory illness suspected to be COVID-19, as his family members also had similar symptoms. At the time, there was no history of drug use or recent vaccination.
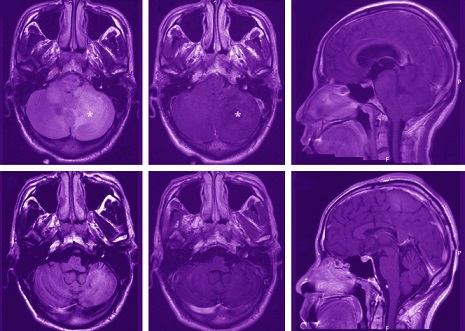
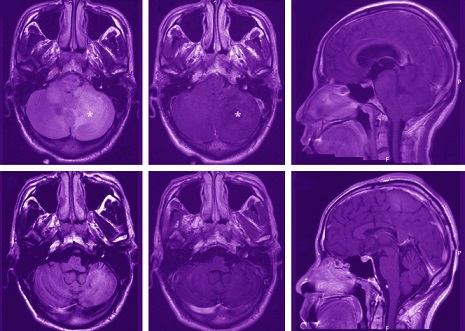
Despite the severity of his symptoms, routine laboratory findings were normal. This included a C-reactive protein (CRP) level of just 0.14 mg/dL, which ruled out acute inflammation. Two COVID-19 PCR tests were weakly positive, confirming a recent SARS-CoV-2 infection. However, brain imaging scans, including computed tomography (CT) and magnetic resonance imaging (MRI), showed no abnormalities. Cerebrospinal fluid (CSF) analysis revealed no significant infection or inflammation, further puzzling the doctors.
Diagnosing Acute Cerebellitis
Initially, the medical team suspected a common viral or bacterial infection affecting the brain, but the normal test results contradicted this theory. When the patient's cerebellar syndrome worsened on the third day, including worsening speech problem
s and severe ataxia, a second round of testing was conducted. This time, a slight increase in CSF protein was noted, but other indicators remained within normal limits.
Given the lack of clear infectious signs, the doctors hypothesized that the patient’s cerebellitis was immune-mediated - a reaction triggered by the patient’s immune system rather than a direct viral invasion of the brain. Post-infectious immune responses are becoming increasingly recognized as potential complications of COVID-19. Thus, the team made the critical decision to start early treatment with high doses of intravenous (IV) steroids, a common treatment for immune-mediated brain inflammation.
The Treatment Approach
On day four of his hospital stay, the patient was started on a high dose of methylprednisolone, a potent steroid, to reduce brain inflammation. Antibiotics, initially given as a precaution, were discontinued once the test results confirmed no bacterial infection. By day seven, the patient’s condition had worsened further, and he was transferred to the intensive care unit (ICU) due to difficulties swallowing, putting him at risk of choking or aspiration pneumonia. His neurological symptoms were now life-threatening, with his ataxia measured as severe.
At this critical point, IV immunoglobulin therapy (IgIV) was initiated to help regulate his immune system and reduce inflammation. Over the next few days, his symptoms began to improve. A whole-body PET scan to check for underlying causes of inflammation came back normal, providing relief to the medical team.
A Remarkable Recovery
By day nine, the patient was moved out of the ICU and back to the neurology ward, showing significant improvement. His ataxia was improving, and follow-up brain scans were still clear, with no signs of permanent damage. After 30 days in the hospital, the patient was transferred to a rehabilitation center to help with his remaining mild speech and coordination issues. Just a week later, he was fully discharged with no significant symptoms remaining, except for slight dysphonia (a mild voice disorder). By day 37, even his speech had returned to normal, and his full recovery was confirmed.
The doctors monitored the patient for five months, during which time he showed no signs of relapse or lasting neurological damage.
Why Early Treatment Matters
This case highlights the critical need for early treatment in post-COVID cerebellitis, even when tests appear normal. The team emphasized that delayed treatment could have resulted in permanent neurological damage or a slower recovery. The use of high-dose steroids and immunoglobulin therapy in the early stages proved essential for this patient’s recovery.
Although this condition is rare, it’s becoming increasingly recognized that SARS-CoV-2 can trigger immune reactions in the brain even after the acute phase of infection has passed. This post-infectious phase can occur several days to weeks after the initial infection. For doctors, this means that COVID-19-related acute cerebellitis (AC) must always be considered when a patient presents with sudden, severe neurological symptoms.
Studies of similar cases have shown that the faster doctors can initiate steroids and immunoglobulins, the better the outcomes for the patient. According to Dr. Klopfenstein and his team, late treatment (after day 7 of symptoms) could lead to incomplete recovery or long-term neurological issues.
A Complex Diagnosis
One of the most alarming aspects of this case is the way it challenges the typical diagnostic process. The patient’s test results, including CSF analysis, MRI, and EEG, were all normal, yet he was experiencing severe, life-threatening neurological symptoms. This kind of situation requires doctors to be vigilant and consider cerebellitis even when no clear cause is identified through initial tests.
Normal imaging and test results do not always rule out serious conditions. In the patient’s case, it was the clinical presentation - his inability to speak properly, walk, and maintain balance—that guided the treatment plan, not the diagnostic tests.
Conclusions
This case serves as a strong reminder to medical professionals that COVID-19 can have serious post-infectious neurological complications. The key takeaway from this case is the importance of clinical judgment. Even in the face of normal test results, the medical team decided to proceed with aggressive treatment due to the severity of the patient’s symptoms. Their decision ultimately saved the patient from potentially irreversible brain damage. The study reinforces the need for early intervention with steroids and immunoglobulin therapy to improve outcomes in acute cerebellitis cases.
For everyday people, this case reminds us that COVID-19 is still a serious disease that can lead to unexpected complications long after recovery. While the majority of cases result in mild symptoms, the risk of rare complications like cerebellitis exists and should be taken seriously.
The study findings were published in the peer-reviewed journal: Infectious Diseases and Therapy.
https://link.springer.com/article/10.1007/s40121-024-01048-4
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/texas-scientist-warns-of-new-sars-cov-2-neuroinvasion-pathway-involving-the-trigeminal-nerve
https://www.thailandmedical.news/news/study-review-validates-that-covid-19-causes-a-variety-of-neuropsychological-issues
https://www.thailandmedical.news/news/covid-19-s-hidden-impact-enlarged-brain-structures-in-some-patients