For The Latest Medical News, Health News, Research News, COVID-19 News, Pharma News, Glaucoma News, Diabetes News, Herb News, Phytochemical News, Thailand Cannabis News, Cancer News, Doctor News, Thailand Hospital News, Oral Cancer News, Thailand Doctors
Various studies have shown people with fibromyalgia see many doctors before receiving an accurate diagnosis. Even with doctors who understand fibromyalgia, other diseases must be ruled out before looking at a fibromyalgia diagnosis. And because some doctors still don’t believe a patient’s pain and symptoms are real, it may take time to find a doctor who will actually listen and take the time determine the truth behind a patient’s symptoms.
Doctors and researchers don’t consider fibromyalgia a disease. They view it as a syndrome, which - as defined by Merriam Webster Dictionary – is “a group of signs and symptoms that occur together and characterize a particular abnormality or condition.”
Several rheumatic diseases have symptoms similar to fibromyalgia, including rheumatoid arthritis, lupus, ankylosing spondylitis, Lyme disease, and polymyalgia rheumatic. Mental health disorders, (i.e. depression) and neurological disorders, (i.e. multiple sclerosis) can also mimic the symptoms of fibromyalgia.
The main symptoms of fibromyalgia are pain, fatigue, and sleep disturbances. Doctors must rule out other possible reasons for a patient’s symptoms before even considering fibromyalgia. Further, symptoms and their severity vary for each person and change over time.
There are no specific lab tests for fibromyalgia, but a doctor who is educated about the disorder can make a diagnosis based on the criteria set by the American College of Rheumatology (ACR), which currently involves a medical history of widespread pain lasting beyond 3 months, tenderness and some common symptoms. The ACR recognizes widespread pain, as pain felt on both sides of the body, as well as above and below the waist.
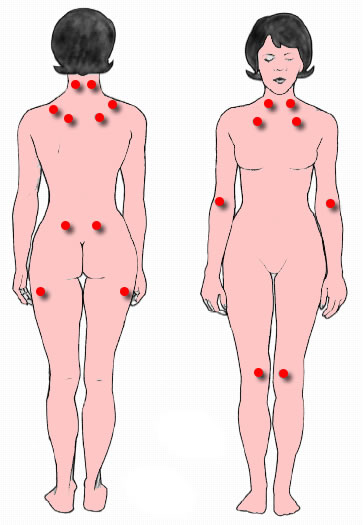 |
| The location of the nine paired tender points that comprise the 1990 American College of Rheumatology criteria for fibromyalgia. |
In 1990, the American College of Rheumatology (ACR), established the first fibromyalgia diagnostic criteria, involving physical examination of specific tender points on the body. That report was published in the February 1990 journal of Arthritis and Rheumatism.
A diagnosis of fibromyalgia, based on the 1990 criteria, was made if a patient had at least 11 of 18 tender points and pain lasting more than 3 months on both sides of the body, as well as above and below the waist. No fibromyalgia symptoms were considered in the original diagnostic criteria and while other diseases were ruled out by doctors, exclusion was not part of the old criteria.
The tender points’ method is now considered ineffective as fibromyalgia pain varies (i.e., a person may have eleven tender points one day and only six the next). And doctors were uncertain how much pressure to apply during the tender point exam, while others weren’t willing to make a diagnosis of fibromyalgia based on tender points alone, as reported by researchers in the February 2010 Arthritis Care & Research journal, wherein the 2010 criteria was first introduced.
The 2010 diagnostic criteria was updated in 2011 and most recently, in 2016. The 2010 fibromyalgia diagnostic criteria removed the 18 tender points examination standard, changed the fibromyalgia definition, gave widespread pain numerical measures via a widespread pain index (WPI), incorporated fibromyalgia’s many symptoms, created a symptom severity chart, and gave fibromyalgia acknowledgement as a real medical condition.
The most recent updates to the ACR's diagnostic criteria were reported at the annual meeting in September 2016. This new update allows for a diagnosis based on generalized pain in 4 of 5 regions and other symptoms, lasting for at least three months. Symptoms considered in diagnosis include, but are not limited to, fatigue, un-refreshed sleep, cognitive issues, dizziness, numbness and tingling, nausea, chest pain, ringing in ears, dry eyes, and easy bruising. The entire list of symptoms can be found in the February 2010 Arthritis Care & Research report.
The 2016 updated criteria also made changes to the widespread pain index (WPI) and a symptom severity scale (SSS) numbers. Finally, the language on ruling out other diseases was modified to acknowledge fibromyalgia could coexist with other diseases.
Once all other health conditions have been ruled out with lab work and other diagnostic testing, and nothing explains pain and symptoms, a doctor can consider a fibromyalgia diagnosis.
Prior to diagnosis, patients generally undergo a physical exam, with the patient alerting the doctor of specific areas on the body causing pain and their severity. These areas are part of the widespread pain index (WPI), and include 19 areas on both sides of the body. Each pain area is given one point, the total score ranging from 0 to 19.
The doctor will also ask about other symptoms, most notably, sleep issues, cognitive issues, and extreme fatigue. These symptoms are ranked on scale of 0 to 3, where the patient is asked how much a symptom has affected the patient over the past week.
According to the ACR 2016 updated diagnostic criteria for fibromyalgia, a diagnosis can be considered if scores include both a widespread pain index (WPI) of 7 or more, and a symptom severity scale (SSS) of 5 or more; OR a WPI of 4 to 6 and a SSS of greater than 9.
Since fibromyalgia has a genetic component, a doctor may also ask if other relatives have fibromyalgia or similar symptoms.
Because there is no diagnostic testing - just criteria - fibromyalgia will continue to remain a diagnosis of exclusion. Doctors will need to continue to diagnose patients based on their descriptions of pain and symptom severity.