Nikhil Prasad Fact checked by:Thailand Medical News Team Sep 19, 2024 1 year, 4 months, 1 week, 3 days, 4 hours, 8 minutes ago
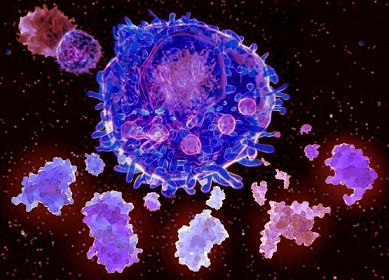
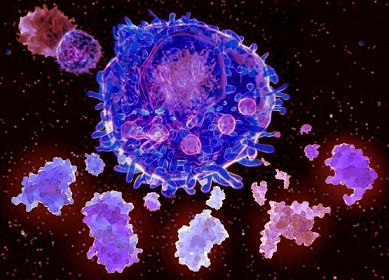
Medical News: The COVID-19 pandemic has led to a significant focus on understanding the virus's behavior and its effects on the human immune system. While the virus affects people differently, one of the major complications seen in severe cases is a condition known as Cytokine Release Syndrome (CRS). CRS can result in a life-threatening inflammatory response, leading to organ damage and even death. Recently, a team of researchers from Jilin University, China, made significant strides in understanding how the SARS-CoV-2 spike protein triggers this dangerous immune reaction by stimulating the body's immune cells, especially T cells, to produce more interleukin-2 (IL-2), a cytokine heavily involved in CRS.
 How T cells and IL-2 drive dangerous immune reactions in COVID-19
The Study: Key Findings
How T cells and IL-2 drive dangerous immune reactions in COVID-19
The Study: Key Findings
The study, led by researchers from Jilin University’s Cancer Center, International Center of Future Science, and the Cancer Research Institute, provides insight into how the spike protein of SARS-CoV-2 may trigger CRS. Specifically, the research shows that the spike protein works alongside IL-2 to stimulate human peripheral blood mononuclear cells (PBMCs) to release high levels of inflammatory cytokines, including IL-1β, IL-6, and IL-8. The combination of IL-2 and spike protein triggers a more intense immune response, which can escalate the severity of symptoms in COVID-19 patients, particularly those experiencing severe illness.
According to the researchers, dendritic cells that are loaded with the SARS-CoV-2 spike protein stimulate T cells to release large amounts of IL-2. This leads to a cascading effect: the IL-2 released by the T cells interacts with the spike protein to encourage PBMCs to produce additional inflammatory cytokines. Natural killer (NK) cells, another type of immune cell, are also activated and release tumor necrosis factor-alpha (TNF-α) and interferon-gamma (IFN-γ). Together, these cytokines enhance the production of inflammatory mediators, further amplifying the body’s immune response.
The Dangerous Cascade
The study reveals that IL-2 plays a critical role in worsening inflammation. When combined with the spike protein, IL-2 not only boosts the production of cytokines but also activates NF-kB, a key transcription factor in monocytes that drives the production of inflammatory cytokines. This
Medical News report will explore the intricate interactions between IL-2, spike protein, and immune cells, which may explain why some COVID-19 patients experience overwhelming immune responses, leading to severe CRS.
When dendritic cells present the spike protein to T cells, the immune system's response goes into overdrive. The T cells then release IL-2, which further activates NK cells and monocytes, encouraging them to produce even more cytokines like TNF-α and IFN-γ. These cytokines are key players in the body’s immune defense, but when released in excess, they can cause damage to organs and tissues, as is seen in severe cases of COVID-19.
How D
oes the Spike Protein Interact with IL-2?
The research demonstrates that the spike protein of SARS-CoV-2 binds to pattern recognition receptors like toll-like receptor 4 (TLR4) on the surface of immune cells such as monocytes. This binding interaction triggers a chain reaction, activating NF-kB, a protein complex that controls the transcription of DNA and the production of cytokines. When the spike protein interacts with IL-2, this process is amplified, leading to even more significant production of inflammatory cytokines.
This interplay between the spike protein and IL-2 may help explain why some patients experience such severe immune responses even when the viral load is not excessively high. It appears that the presence of the spike protein, combined with an overactive immune response driven by IL-2, is enough to tip the balance toward a potentially fatal inflammatory reaction.
Implications for COVID-19 Treatment
The findings of this study highlight the importance of targeting specific cytokines and immune pathways to mitigate CRS in COVID-19 patients. The researchers suggest that therapies aimed at blocking TNF-α and IFN-γ, in combination with inhibiting TLR4 signaling, could be an effective strategy for preventing or treating severe CRS. These targeted interventions could help reduce the excessive inflammatory response seen in critically ill patients, providing a potential lifeline for those most at risk.
By targeting these pathways, it may be possible to prevent the immune system from spiraling out of control. The combination of TNF-α and IFN-γ, when stimulated by IL-2 and spike protein, is critical to the activation of monocytes and the release of dangerous levels of inflammatory cytokines. Reducing the activity of these molecules could help prevent the progression of CRS and improve outcomes for patients with severe COVID-19.
Why This Study Matters
This study provides a new perspective on how the SARS-CoV-2 virus interacts with the immune system to cause severe disease. By focusing on the role of IL-2 and its interaction with the spike protein, the research sheds light on the underlying mechanisms that drive CRS. Understanding these mechanisms is crucial for developing more effective treatments for COVID-19, particularly for those patients who experience severe immune reactions.
The insights gained from this research could also have broader implications for other diseases and conditions associated with CRS, including certain types of cancer treatments. By exploring the pathways involved in CRS, researchers may be able to develop therapies that can be applied to a range of inflammatory diseases beyond COVID-19.
Conclusions
In conclusion, this groundbreaking study from Jilin University highlights the significant role of IL-2 in amplifying the body’s immune response when it interacts with the SARS-CoV-2 spike protein. The research suggests that this interaction may be responsible for triggering the severe inflammatory reactions seen in patients with CRS, which can lead to life-threatening complications such as organ failure.
Targeting the pathways involved in this immune response, particularly TNF-α, IFN-γ, and TLR4 signaling, may offer new therapeutic options for preventing or treating CRS in COVID-19 patients. These findings provide a critical foundation for future research aimed at understanding how to control the immune system’s response to SARS-CoV-2, potentially saving lives and improving outcomes for those affected by severe COVID-19.
The study findings were published in the peer-reviewed journal: Frontiers in Immunology.
https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1444643/full
For the latest COVID-19 News, keep on logging in to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/unknown-to-many-including-doctors-covid-19-causes-parsonage-turner-syndrome
https://www.thailandmedical.news/news/doctors-warn-that-covid-19-can-cause-spontaneous-esophageal-rupture
https://www.thailandmedical.news/news/australian-study-reveals-that-many-post-covid-19-individuals-develop-cardiac-function-impairment
https://www.thailandmedical.news/news/new-approach-identifies-antibody-resistant-covid-19-mutations