BREAKING! SARS-CoV-2 Mutations: Washington University, Mayo and Harvard Scientist Identify New 48 SARS-CoV-2 RBD Mutations Resistant To Antibodies!
Source: SARS-CoV-2 Mutations Nov 11, 2020 5 years, 2 months, 2 weeks, 6 days, 16 hours, 46 minutes ago
SARS-CoV-2 Mutations: Researchers from Washington University-St. Louis, Harvard Medical School and Mayo Clinic in a new study using a variety of monoclonal antibodies (mAbs) to understand the mutational landscape of resistance in the SARS-CoV-2 receptor-binding domains (RBD) have discovered 48 new mutations resistant to antibodies including 27 that are circulating in humans.
.jpg) More worrisome is the fact that about 86 % of all isolates from the D614G strains that is currently most prevalent, have been found to have these antibody resistant mutations on them.
More worrisome is the fact that about 86 % of all isolates from the D614G strains that is currently most prevalent, have been found to have these antibody resistant mutations on them.
These newly discovered mutations can have massive implications on the vaccine and antibody therapeutics developments underway and also is issuing warning signals about the recently approved monoclonal protocol by the U.S. FDA and also all future monoclonal or cocktail antibody treatment protocols.
In the study, the most worrisome mutation was the E484 as it was to be resistant to neutralization by most sera. Another mutation that was also of concern was the S477 mutation especially the S477N emerging strains.
Although neutralizing antibodies against the SARS-CoV-2 spike (S) protein are a goal of most COVID-19 vaccines and being developed as therapeutics, escape mutations could compromise such countermeasures. To define the immune-mediated mutational landscape in S protein, the study team used a VSV-eGFP-SARS-CoV-2-S chimeric virus and 19 neutralizing monoclonal antibodies (mAbs) against the receptor binding domain (RBD) to generate 48 escape mutants. These variants were mapped onto the RBD structure and evaluated for cross-resistance by convalescent human plasma. Although each mAb had unique resistance profiles, many shared residues within an epitope, as several variants were resistant to multiple mAbs. Remarkably, we identified mutants that escaped neutralization by convalescent human sera, suggesting that some humans induce a narrow repertoire of neutralizing antibodies. By comparing the antibody mediated mutational landscape in S protein with sequence variation in circulating SARS-CoV-2 strains, we identified single amino acid substitutions that could attenuate neutralizing immune responses in some humans.
The study findings were published on a preprint server and are currently being peer reviewed.
https://www.biorxiv.org/content/10.1101/2020.11.06.372037v1
Utilizing a set of different monoclonal antibodies, the study team determined different mutations in the SARS-CoV-2 spike protein that leads to resistance. Understanding these resistant mutations is important in developing effective therapeutic strategies.
The SARS-CoV-2 coronavirus, responsible for the COVID-19 pandemic, infects host cells via the spike proteins on the virus surface. The N-terminal subunit (S1) plays a role in receptor binding and the C-terminal subunit (S2) helps in the virus-host cell membrane fusion.
It has been found that the receptor-binding domains (RBDs) of S1 bind to the human angiotensin-converting enzyme 2 (ACE2). SARS-CoV-2 antibodies prevent infection by targeting the RBD.
It has long been known that RNA viruses, like SARS-CoV-2, are present as a swarm of genome sequences
around a core sequence. Variants can escape from this swarm in the presence of antibodies or drugs and become resistant.
At present there are now more than 2,700 mutations identified in the spike protein of the SARS-CoV-2 virus. There may be several mechanisms for these mutations, like host adaptation and immune selection during natural infection.
Importantly additional mutants could arise with the use of vaccines, therapeutic antibodies, and convalescent plasma therapy, which may reduce the effectiveness of these therapies.
In fact in the current pandemic, Thailand Medical News strongly believes in the hypothesis that many of the current emerging antibody resistant mutations are emerging as a result of the wrong usage of convalescent plasma protocols used by ignorant medical professionals and researchers and also the introduction of monoclonal and cocktail antibodies protocols by greedy biotech companies. (Most are proving to be ineffective in treating COVID-19 and are only contributing to the growing resistance not to mention of future dangers of ADE Antibody-dependent enhancement ). We also strongly believe that most of the vaccines under developments once introduced to the masses will backfire badly as the pandemic takes on a new dimension and kinetics with the growing emergence of more variants and mutations and the rise of reinfections, co-infections and ‘zoonotic back infections’.
In this study, the study team used a chimeric infectious vesicular stomatitis virus (VSV), a SARS-CoV-2 mimic, where they replaced the glycoprotein with the SARS-CoV-2 spike protein. Using the mAb 2B04, the team determined that SARS-CoV-2 variants that were not neutralized had mutations in the RBD related to residues involved in ACE2 binding.
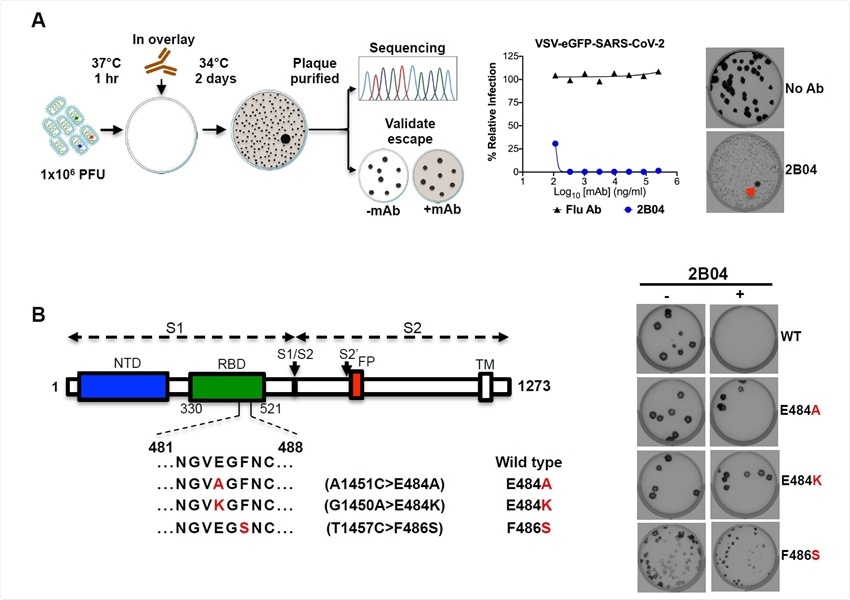
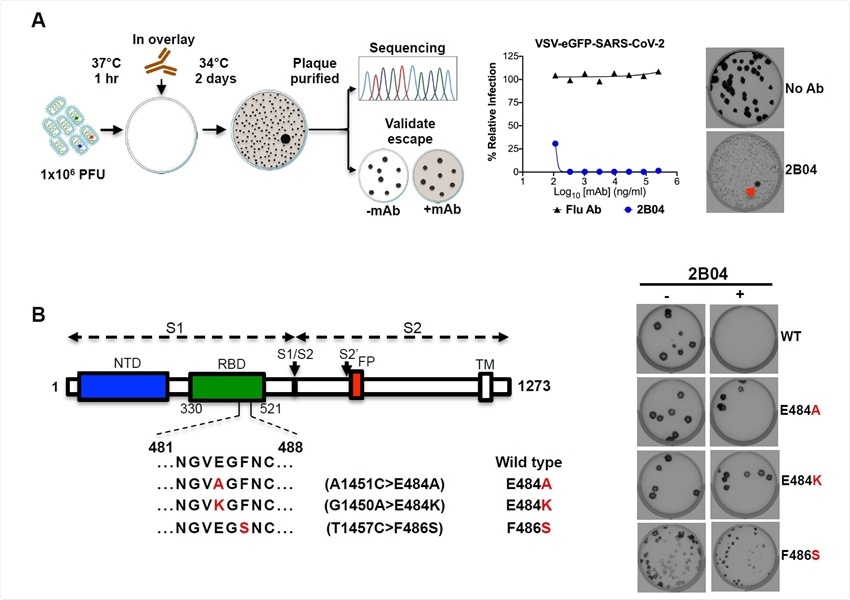 VSV-SARS-CoV-2 escape mutant isolation. (A) Outline of escape mutant selection experiment. 2B04 and a control anti-influenza mAb were tested for neutralizing activity against VSV-SARS-CoV-2. The concentration of 2B04 added in the overlay completely inhibited viral infection (middle panel). Data are representative of two independent experiments. Plaque assays were performed to isolate the VSV-SARS-CoV-2 escape mutant on Vero E6 TMPRSS2 cells (red arrow indicated). Plaque assays with 2B04 in the overlay (Bottom plaque in the right panel); plaque assays without Ab in the overlay (Top plaque in the right panel). Data are representative images of three independent experiments. (B) Schematic of S gene, which underwent Sanger sequencing to identify mutations (left panel). For validation, each VSV SARS-CoV-2 mutant was tested in plaque assays with or without 2BO4 in the overlay on Vero cells (right panel). Representative images of two independent experiments are shown.
VSV-SARS-CoV-2 escape mutant isolation. (A) Outline of escape mutant selection experiment. 2B04 and a control anti-influenza mAb were tested for neutralizing activity against VSV-SARS-CoV-2. The concentration of 2B04 added in the overlay completely inhibited viral infection (middle panel). Data are representative of two independent experiments. Plaque assays were performed to isolate the VSV-SARS-CoV-2 escape mutant on Vero E6 TMPRSS2 cells (red arrow indicated). Plaque assays with 2B04 in the overlay (Bottom plaque in the right panel); plaque assays without Ab in the overlay (Top plaque in the right panel). Data are representative images of three independent experiments. (B) Schematic of S gene, which underwent Sanger sequencing to identify mutations (left panel). For validation, each VSV SARS-CoV-2 mutant was tested in plaque assays with or without 2BO4 in the overlay on Vero cells (right panel). Representative images of two independent experiments are shown.
Detailed testing with nine other mAbs revealed a similar result. For the mAb 2H04, the resistance mutations were present outside the ACE2 binding site, on the side and base of the RBD. This suggests virus neutralization may occur by alternative attachment factors.
Importantly several resistance mutations were common among the different mAbs tested, suggesting they represent important antigenic sites on the RBD.
Interestingly the resistance mutations arising from the different mAbs made them resistant to the other mAbs in the chosen array of mAbs. Substitutions at S477 and E484 led to a broad resistance, while substitutions at several other sites led to resistance to more than one mAb.
Other worrying mutations included F486S, T345, R346, K444, G446, 156 N450, L452, T478, F486 and P499 as each were associated with resistance to more than one mAb.
Also soluble human ACE2 receptors, which are not attached to cells and can compete with those on the host cell to bind to the virus, are another strategy being investigated to combat the virus. The study team tested the resistance of Vero E6 cells to human and murine soluble ACE2. The human soluble ACE2 neutralized all the escape mutants, although some mutations required higher ACE2 concentrations to be neutralized. Several mutants required higher (3-5-fold) concentrations of hACE2 to block infection, including substitutions at T345A, T345N, G446D, G446V, E484D and F486Y.
The study team also used serum from four convalescent COVID-19 patients to test if the serum antibodies neutralized the escape mutant viruses. They found many mutations that were resistant to neutralization by the sera. In particular, the mutation at residue E484 was resistant to all the four sera, suggesting this is a major neutralizing epitope. However, substitution at this position was quite rare and found only in about 0.05% of strains sequenced.
The study team also tested additional mutations, adding up to 48 different escape mutants. The team also investigated if any of these mutants are present in human isolates of SARS-CoV-2 by compiling available genome sequences of the virus and comparing them against the mutants' genome sequence.
They found 27 of the 48 mutations are circulating in humans, with the most frequent mutation seen being D614G, observed in 86% of the isolates.
Most significantly substitution at S477N, which conferred a resistance to some level in all the mAbs, was the second most abundant variant in the human isolates.
The study team noted a few limitations of the study. Although the VSV is an effective mimic of the SARS-CoV-2 virus, 27 escape mutants were found only in the human isolates of the virus. They also note the few human sera tested. More human sera samples may help determine the extent of neutralization and escape mutants present.
Most importantly the study team warned that if such variations in the virus arise after vaccination, they could limit the efficacy of treatment.
The study team said, "The relatively low genetic barrier to resistance combined with knowledge of the presence of relevant substitutions in clinical isolates suggests that effective mAb therapy likely will require a combination of at least two neutralizing antibodies,"
Determining the residues resistant to specific antibodies could help select combinations based on non-overlapping resistant mutations.
The study team warns that the international research community should pay detailed attention to not only these antibody resistant mutations but also newer mutations fast emerging in the prevailing circulation.
Thailand Medical News would also like to note that there seems to be a concerted effort by the US agencies like NIH, CDC FDA and even by the WHO and the various pharmaceutical and biotech giants to either ignore or downplay all these emerging SARS-CoV-2 variants and mutated strains that are antibody resistant despite many of them gaining dominance in circulation. Sadly as there is trillions of dollars at stake in many of these vaccine and antibody therapeutic programmes, media, resarchers and medical journals are being bought to downplay what could be a coming disaster as the COVID-19 pandemic evolves and is expected to remain for the next few years.
Read also:
https://www.thailandmedical.news/news/covid-19-mutations-international-study-warns-of-more-strains-emerging-that-can-evade-human-immune-response,-new-n439k-mutation-is-a-concern--
For more on
SARS-CoV-2 Coronavirus, keep on logging to Thailand Medical News.
.jpg)