BREAKING! Peer Reviewed Published Swedish Study Shows That IgA Antibodies In Respiratory Tract Can Protect The Unvaccinated Against COVID-19!
Source: Medical News - COVID-19 Immunology Mar 25, 2022 3 years, 10 months, 5 days, 10 hours, 15 minutes ago
COVID-19 Immunology: A new study by Swedish researchers from University of Gothenburg, Sahlgrenska University Hospital and the Nötkärnan Primary Health Care Center Consortium has found that IgA Antibodies in respiratory tract can protect the unvaccinated against COVID-19!
The research involved the detailed study of the patterns of humoral and cellular responses to SARS-CoV-2 in unvaccinated Swedish primary health care workers (n = 156) for 6 months during the COVID-19 pandemic.
The
COVID-19 Immunology study team monitored serum IgA and IgG to SARS-CoV-2, T-cell proliferation and cytokine secretion, demographic and clinical data, PCR-verified infection, and self-reported symptoms in all the participants.
Furthermore, the multivariate method OPLS-DA was used to identify immune response patterns coupled to protection from COVID-19.
Typically contracting COVID-19 was associated with SARS-CoV-2-specific neutralizing serum IgG, T cell, IFN-γ, and granzyme B responses to SARS-CoV-2, self-reported typical COVID-19 symptoms, male sex, higher BMI, and hypertension. Not contracting COVID-19 was associated with female sex, IgA-dominated, or no antibody responses to SARS-CoV-2, airborne allergy, and smoking.
The IgG-responders had SARS-CoV-2-specific T-cell responses including a cytotoxic CD4+ T-cell population expressing CD25, CD38, CD69, CD194, CD279, CTLA-4, and granzyme B.
Interestingly, IgA-responders with no IgG response to SARS-CoV-2 constituted 10% of the study population. The IgA responses were partially neutralizing and only seen in individuals who did not succumb to COVID-19.
The study findings showed that serum IgG-dominated responses correlated with T-cell responses to SARS-CoV-2 and PCR-confirmed COVID-19, whereas IgA-dominated responses correlated with not contracting the infection.
The study findings were published in the peer reviewed journal: European Journal Of Immunology.
https://onlinelibrary.wiley.com/doi/10.1002/eji.202149655
It was found that despite daily contact with COVID-19 patients early in the pandemic, some health professionals who were not vaccinated avoided falling ill.
The University of Gothenburg led study shows that a possible explanation appears to be an antidote in the immune system: IgA antibodies to COVID-19.
In order to comprehend how the immune system builds up its defenses against COVID-19, the study team monitored 156 employees at five primary care health centers, belonging to the Nötkärnan group in the Gothenburg area, for six months.
The study participants were recruited during April and May 2020 and none of them had been vaccinated against COVID-19, and most of them met infected patients daily.
It was found that the reason why some of the medical staff did not contract the disease seems to have been that IgA (immunoglobulin A) was present in their respiratory tract.
These IgA antibodies found naturally in the secretions of mucous membranes in the airways and gastroin
testinal tract, can protect the body by binding to viruses and other invading organisms.
The study findings showed that a third of the care workers developed antibodies to COVID-19. These subjects fell into two distinct groups based on antibody patterns and COVID-19 incidence.
The first group had IgA antibodies only, never succumbed to COVID-19.
However, study participants in the other group had both IgG antibodies and T cells, and contracted the disease.
The acquired immune system also includes IgG antibodies and T cells, which serve to recognize viruses, for example, and protect us against them.
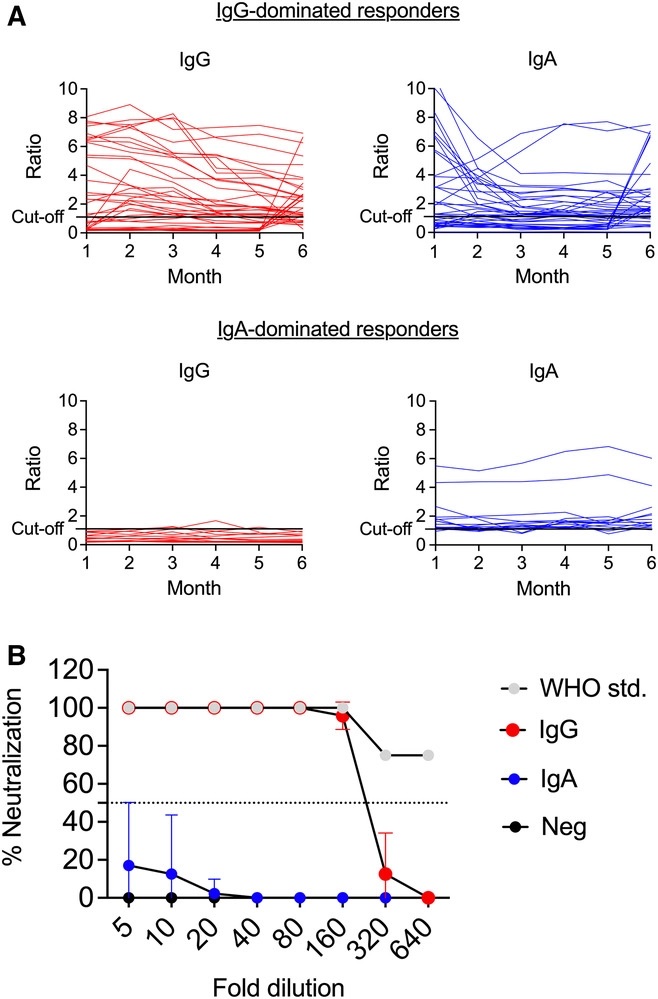
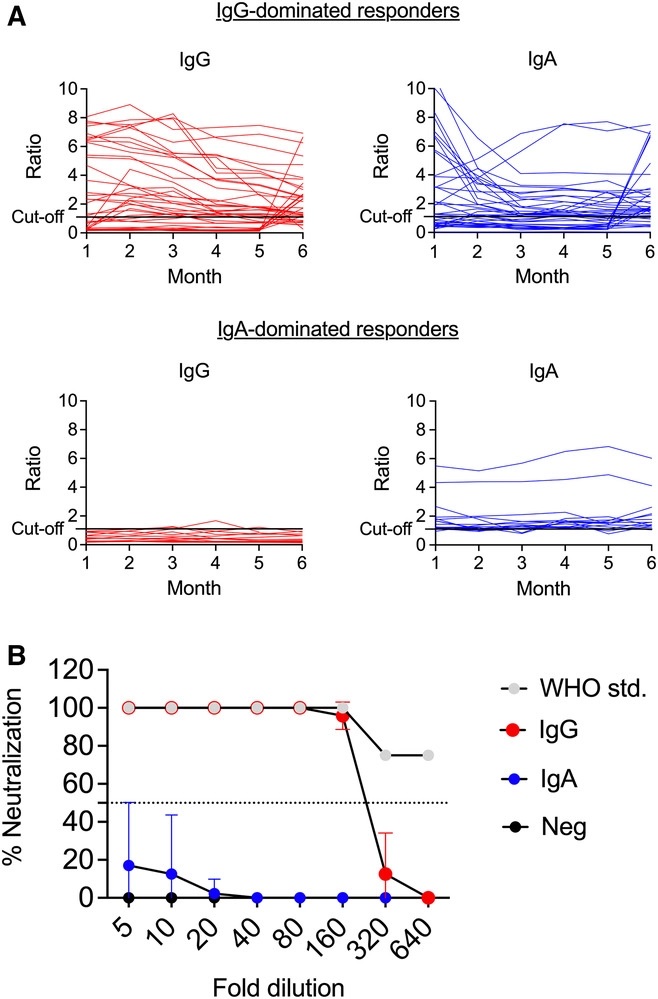 IgG-dominated versus IgA-dominated humoral responses and SARS-CoV-2 neutralizing capacity. (A) Serum samples were collected once a month during a period of 6 months. Levels of IgG and IgA antibodies to SARS-CoV-2 were analyzed using ELISA. Data are presented as ratios, which corresponds to an adjusted OD-value (OD-value of serum sample/OD-value of calibrator), over time in IgG-dominated and IgA-dominated responders. A ratio of ≥1.1 was positive; ≥0.8 to <1.1 borderline; <0.8 negative. (B) Neutralization capacity of sera from patients positive for anti-SARS-CoV-2 IgG (red, n = 3), IgA-dominated responders (blue, n = 11) and from patients with no antibodies against SARS-CoV-2 (black, n = 3) was tested using a live virus PRNT neutralization assay. The WHO anti-SARS-CoV-2 IgG standard (grey) was included as a positive control. Percent antibody-mediated neutralization of the Freiburg SARS-CoV-2 isolate was measured at 10-point twofold serum dilutions (8 points depicted). Data are presented as mean with standard deviation.
IgG-dominated versus IgA-dominated humoral responses and SARS-CoV-2 neutralizing capacity. (A) Serum samples were collected once a month during a period of 6 months. Levels of IgG and IgA antibodies to SARS-CoV-2 were analyzed using ELISA. Data are presented as ratios, which corresponds to an adjusted OD-value (OD-value of serum sample/OD-value of calibrator), over time in IgG-dominated and IgA-dominated responders. A ratio of ≥1.1 was positive; ≥0.8 to <1.1 borderline; <0.8 negative. (B) Neutralization capacity of sera from patients positive for anti-SARS-CoV-2 IgG (red, n = 3), IgA-dominated responders (blue, n = 11) and from patients with no antibodies against SARS-CoV-2 (black, n = 3) was tested using a live virus PRNT neutralization assay. The WHO anti-SARS-CoV-2 IgG standard (grey) was included as a positive control. Percent antibody-mediated neutralization of the Freiburg SARS-CoV-2 isolate was measured at 10-point twofold serum dilutions (8 points depicted). Data are presented as mean with standard deviation.
Senior Co-author Dr Christine Wennerås, a Professor of Clinical Bacteriology at Sahlgrenska Academy, University of Gothenburg, and senior physician at Sahlgrenska University Hospital told Thailand
Medical News, "We all have IgA. It's found on the mucous membranes, and COVID-19 is an infection that spreads via those membranes. We thought it was important to investigate what happened when completely healthy people encountered the coronavirus, before vaccines became available.”
Dr Kristina Eriksson, Professor of Viral Immunology at Sahlgrenska Academy and also senior co-author added, "Of the participants in our study, none whom contracted COVID-19 required hospitalization. A lot of other research has concerned the most seriously ill patients, who have been hospitalized and in need of intensive care."
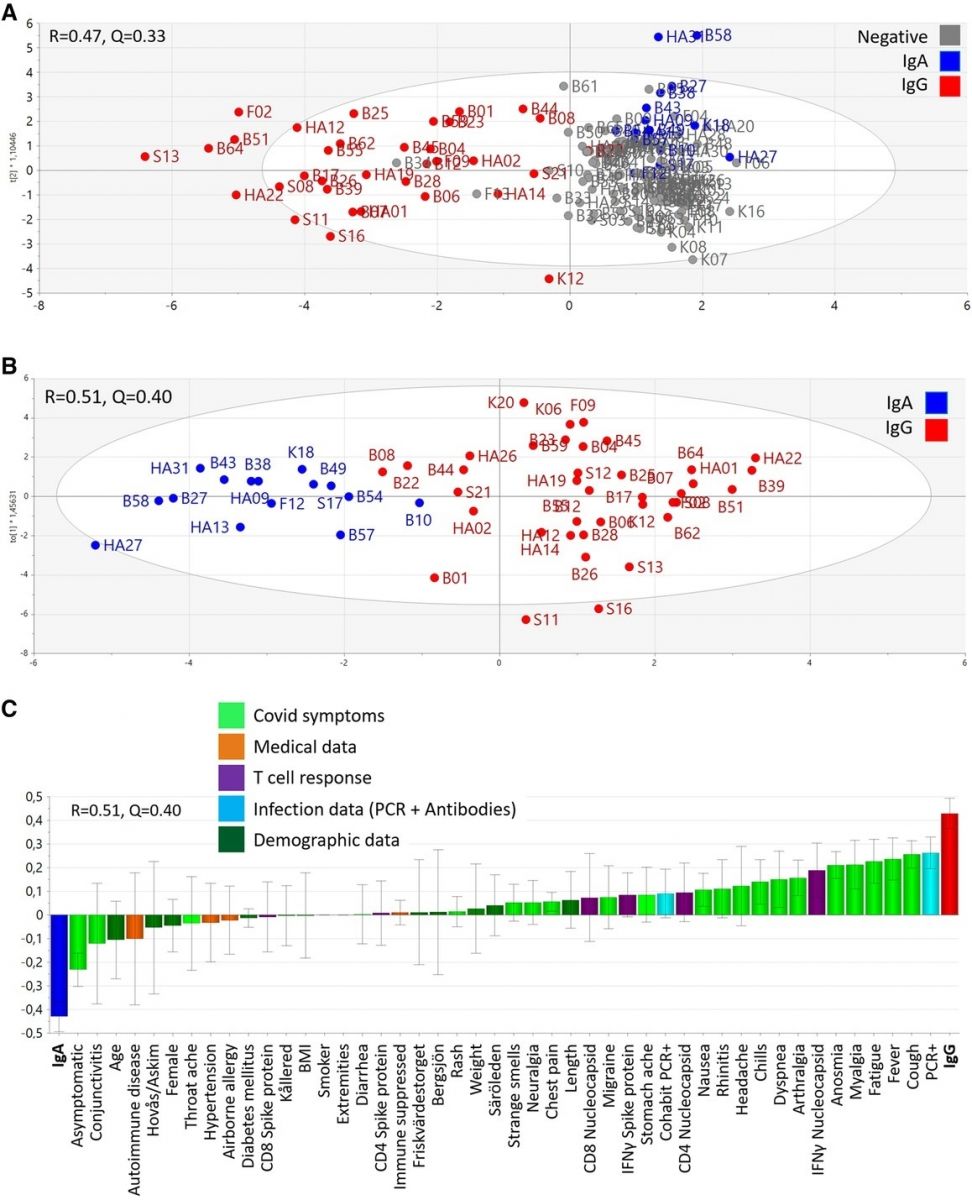
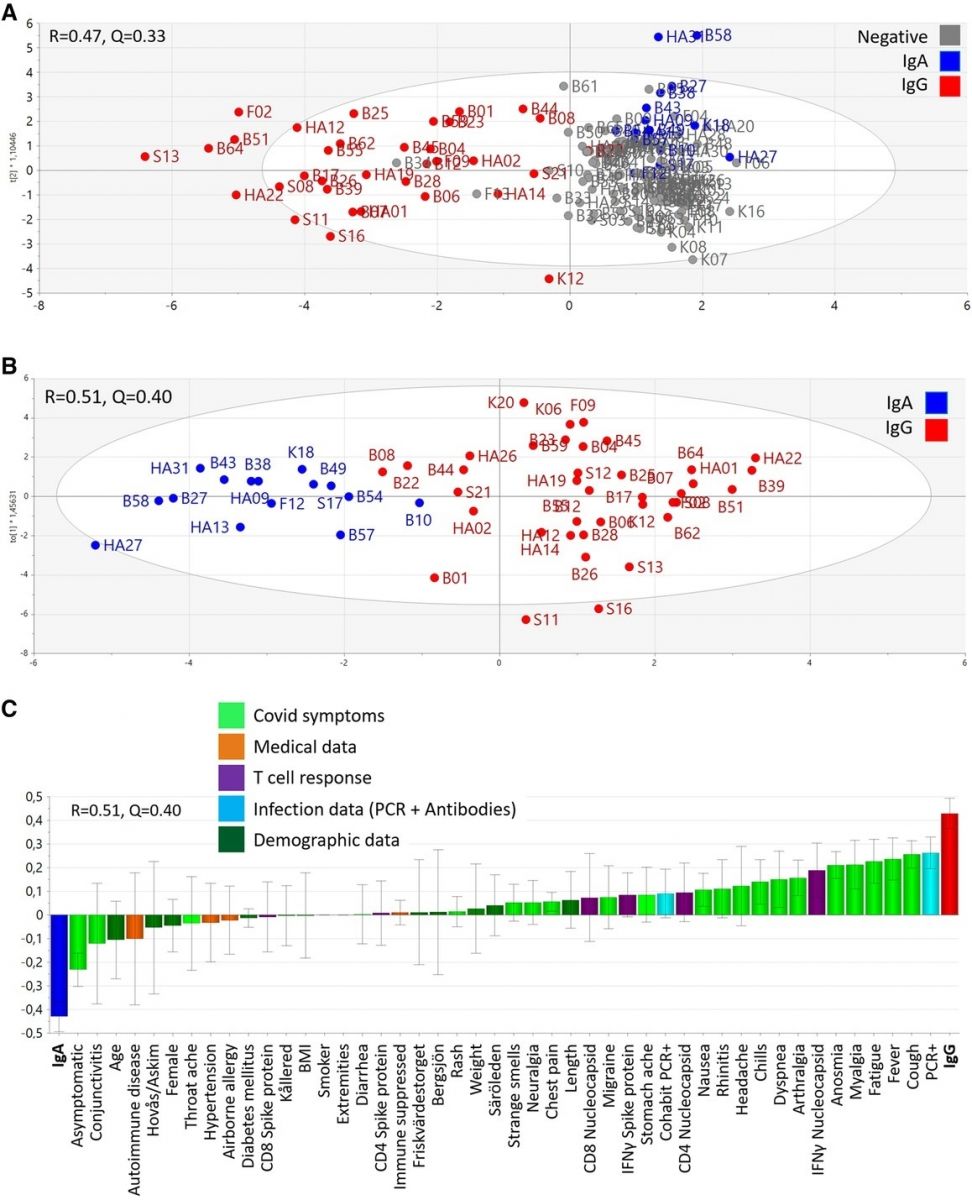 Clustering of individuals with IgG-dominated and IgA-dominated types of antibody responses. The multivariate method “Orthogonal-Projection to Latent Structures Discriminatory Analysis” (OPLS-DA) was used to examine if the study parameters (X-variables) could separate individuals with the various antibody patterns (Y-variables). (A) A multivariate model showing the clustering of individuals with IgG-dominated antibody responses (red, n = 38), IgA-dominated antibody responses (blue, n = 15), and no antibody response (grey, n = 97). Each symbol denotes one individual. The model's stability (Q) and explanatory power (R) is indicated. (B) A multivariate model shows segregation of individuals with the IgG-dominated antibody pattern of response (red, n = 38) from individuals with IgA-dominated antibody response (blue, n = 15). The model's stability (Q) and explanatory power (R) is indicated. (C) A loading plot of the OPLS-DA model depicted in B shows which of the study parameters that had the largest impact on the separation of the IgG-dominated responders from the IgA-only responders. The study parameters (X-variables) were grouped into the categories demographic data (dark green), medical data (orange), infection data (light blue), Covid-19 symptoms (light green) and T-cell responses (purple). Variable bars that are close to and point in the same direction as the bars indicating type of antibody pattern are positively associated with said antibody pattern.
Clustering of individuals with IgG-dominated and IgA-dominated types of antibody responses. The multivariate method “Orthogonal-Projection to Latent Structures Discriminatory Analysis” (OPLS-DA) was used to examine if the study parameters (X-variables) could separate individuals with the various antibody patterns (Y-variables). (A) A multivariate model showing the clustering of individuals with IgG-dominated antibody responses (red, n = 38), IgA-dominated antibody responses (blue, n = 15), and no antibody response (grey, n = 97). Each symbol denotes one individual. The model's stability (Q) and explanatory power (R) is indicated. (B) A multivariate model shows segregation of individuals with the IgG-dominated antibody pattern of response (red, n = 38) from individuals with IgA-dominated antibody response (blue, n = 15). The model's stability (Q) and explanatory power (R) is indicated. (C) A loading plot of the OPLS-DA model depicted in B shows which of the study parameters that had the largest impact on the separation of the IgG-dominated responders from the IgA-only responders. The study parameters (X-variables) were grouped into the categories demographic data (dark green), medical data (orange), infection data (light blue), Covid-19 symptoms (light green) and T-cell responses (purple). Variable bars that are close to and point in the same direction as the bars indicating type of antibody pattern are positively associated with said antibody pattern.
The research focused on identifying health factors that appeared to afford protection against COVID-19. Numerous factors were found by means of extensive questionnaire surveys, blood tests and more. As soon as a participant had nasal congestion, a cough, red eyes, changes in the sense of taste, or anything else that could be an infection, they had to answer questions and undergo a PCR test.
Interestingly, what the subjects who neither tested positive nor fell ill had in common, then, were IgA antibodies, which bind to the coronavirus.
Furthermore, being female and having a respiratory allergy were other factors affording protection against becoming infected. However, the study provides no support for the idea that people without antibodies against COVID-19 have protective T cells.
Dr Wennerås added, "A lot of the COVID-related research has been about IgG antibodies and T cells. The interesting thing is that when we now examine other people's articles and tables, we find evidence for the conclusion we've arrived at about IgA ourselves. But it's not something those studies have highlighted."
A unique finding of the study thought was that contrary to the previous study of Sekine et al., the study team did not find clear-cut antiviral T-cell responses in person without antibodies to SARS-CoV-2 although we used the same SARS-CoV-2-spike protein peptides to stimulate the T cells in vitro.
https://pubmed.ncbi.nlm.nih.gov/32979941/
A likely explanation is that the study team abstained from adding the T-cell growth factor IL-2 and crosslinking the costimulatory molecules CD28/CD49d in the experimental setup.
Another very interesting finding relating to SARS-CoV-2 T-cell responses were the detection of a unique virus-specific cytotoxic CD4+ T-cell population only harbored by individuals who responded with serum IgG to SARS-CoV-2. The virus-specific T-cell population expressed the activation markers CD25, CD38, and CD69, the inhibitory molecules CTLA-4 and CD279 (PD-1), cytotoxic granzyme B, and the chemokine receptor CCR4 (CD194). Upregulation of inhibitory molecules, such as CTLA-4 and PD-1, by a SARS-CoV-2-specific T-cell subset reflects highly activated effector T cells capable of producing large quantities of granzyme B and IFN-γ.
https://pubmed.ncbi.nlm.nih.gov/33784417/
The study team concluded, “Our key findings were that (1) every tenth person had a potentially neutralizing IgA response which was associated with not contracting COVID-19; (2) an IgG response was strongly associated with T-cell responsiveness to SARS-CoV-2 and having contracted COVID-19, and (3) there was scant evidence of T-cell responsiveness to SARS-CoV-2 among seronegative individuals.”
The discovery could lead to the development of COVID-19 prophylactics using IgA based nasal sprays or inhalers.
For more on
COVID-19 Immunology, keep on logging to Thailand
Medical News.