Nikhil Prasad Fact checked by:Thailand Medical News Team Sep 19, 2024 1 year, 4 months, 1 week, 3 hours, 2 minutes ago
Long COVID News: Long-COVID, a condition affecting individuals long after their recovery from an initial SARS-CoV-2 infection, continues to perplex medical researchers. With symptoms that can linger for months, if not years, long-COVID presents as a multi-organ disorder. Those affected often experience a wide range of symptoms, including fatigue, dizziness, shortness of breath, cognitive dysfunction, and joint or muscle pain. According to the National Institute for Health and Care Excellence (NICE) criteria, long-COVID is defined as symptoms lasting more than 12 weeks after infection that cannot be explained by another diagnosis.
 New study finds no link between mast cells and Long-COVID symptoms
New study finds no link between mast cells and Long-COVID symptoms
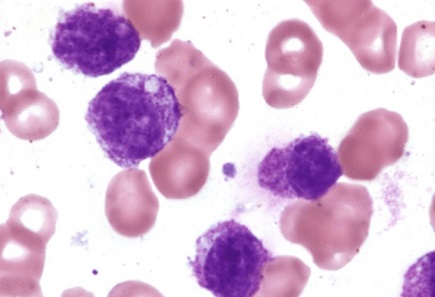
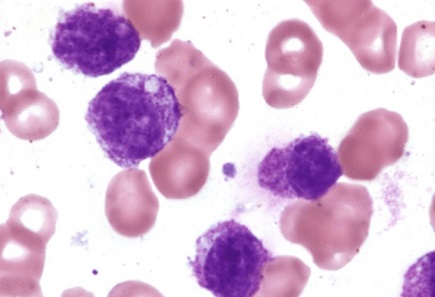
With at least 65 million people globally suffering from these lingering effects, the medical community is desperate for answers. While many studies have proposed mechanisms behind long-COVID, one particular hypothesis has gained attention: the involvement of mast cells, an essential part of the immune system. Mast cells are known to respond to allergens and play a role in the body’s defense against pathogens. Could their activation be driving long-COVID symptoms? A recent study set out to answer this pressing question.
The Study: No Signs of Mast Cell Activation in Long-COVID
A research team led by Ole Bernt Lenning from Stavanger University Hospital and the University of Bergen, Norway, conducted a case-control study to explore the involvement of mast cells in long-COVID. The study measured the levels of two mast cell-specific proteins - beta-tryptase (TPSB2) and carboxypeptidase A3 (CPA3) - in the blood of 24 patients with long-COVID and compared these levels to those of 24 healthy individuals who had recovered from COVID-19 without long-term complications.
This
Long COVID News report aims to provide a detailed breakdown of the study, which did not find any significant evidence of mast cell activation in patients with long-COVID, challenging earlier assumptions. The study is particularly significant because of its focus on two well-known markers of mast cell activation and their potential links to long-COVID symptoms, especially exercise intolerance and fatigue.
How the Study Was Conducted
Participants in the study were recruited from the Stavanger community, with patients diagnosed with long-COVID according to the NICE criteria. Control participants were healthy individuals with a confirmed history of SARS-CoV-2 infection but no lingering symptoms. Blood samples were collected from all participants and analyzed for the presence of TPSB2 and CPA3 using highly sensitive immunoassays.
The inclusion criteria for the study were strict, ensuring a balanced group of participants. Patients ranged in age from 16 to 80, and both groups were matched for age and sex. The exclusion criteria ruled out any participants with autoimmune or chronic inflammatory diseases, cancer, or untreated conditions known to cause fatigue.
The study also explored potential correlations between the levels of TPSB2 and CPA3 and
physical exertion intolerance, a common complaint among long-COVID patients. Researchers used the Physical Functioning Scale of the Short Form-36 Health Survey (SF-36) as a proxy for measuring exercise intolerance.
Key Findings: No Elevated Mast Cell Markers in Long-COVID Patients
The study’s findings were clear: there were no significant differences in the levels of TPSB2 or CPA3 between the long-COVID group and the control group. TPSB2 levels in long-COVID patients had a median value of 26.9 ng/mL, compared to 10.9 ng/mL in the control group, but this difference was not statistically significant. Similarly, CPA3 levels were nearly identical in both groups, with a median of 5.8 ng/mL in long-COVID patients versus 5.3 ng/mL in controls.
Additionally, no correlations were found between TPSB2 or CPA3 levels and measures of exercise intolerance. Despite some initial associations between high TPSB2 and CPA3 levels and low scores on the SF-36 physical subscales (which suggest reduced tolerance for physical activity), these findings did not hold up after statistical corrections were applied.
The Implications: What Does This Mean for Long-COVID Research?
The absence of elevated mast cell markers in long-COVID patients suggests that mast cell activation is not a significant factor in the long-term pathogenesis of the condition. Earlier studies that linked mast cells to post-acute COVID syndrome focused on shorter observation periods, typically around two months. In contrast, the present study followed patients for an average of 60 weeks after their initial COVID diagnosis.
This extended follow-up period provides a clearer picture of the long-term effects of COVID-19 and suggests that mast cell activation, while it may play a role in the early stages of the disease, does not contribute to the prolonged symptoms seen in long-COVID patients. These findings stand in contrast to some previous research that indicated elevated mast cell markers in patients with post-acute COVID-19 syndrome, highlighting the need for further investigation into the different phases of the disease.
Why Exercise Intolerance and Fatigue Persist in Long-COVID
One of the key symptoms of long-COVID is exercise intolerance, where patients report worsening symptoms such as pain, fatigue, and mental fog following physical exertion. This phenomenon is not unique to long-COVID; it is also observed in conditions like chronic fatigue syndrome and fibromyalgia. Some researchers hypothesize that this could be related to abnormalities in the body’s response to mechanical stress, potentially involving mast cells.
However, this study found no evidence that mast cells are responsible for exercise intolerance in long-COVID. Despite this, the researchers acknowledge that exercise-induced malaise remains a major issue for many patients and requires further study. They speculate that the persistence of fatigue and other symptoms may be related to other immune or non-immune mechanisms, possibly involving neuroinflammation or metabolic dysfunction.
Conclusion: A Step Forward in Understanding Long-COVID
The results of this study provide valuable insight into the underlying mechanisms of long-COVID. While mast cells have been implicated in various immune responses, this study suggests that they do not play a significant role in the long-term symptoms experienced by those with long-COVID. The lack of elevated TPSB2 and CPA3 levels in long-COVID patients, along with the absence of significant correlations with exercise intolerance, challenges previous theories about mast cell involvement in the condition.
Moving forward, researchers will need to explore other potential mechanisms behind long-COVID, such as viral reservoirs, autoimmune responses, or neuroimmune dysregulation. By ruling out mast cell activation as a major factor, this study helps narrow the focus of future research and brings us one step closer to understanding the complex nature of long-COVID.
The study findings were published in the peer-reviewed Scandinavian Journal of Immunology.
https://onlinelibrary.wiley.com/doi/10.1111/sji.13407
For the latest Long COVID News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/could-human-lung-mast-cells-be-reservoirs-for-sars-cov-2
https://www.thailandmedical.news/news/the-role-of-mast-cells-in-sars-cov-2-induced-neuroinflammation
https://www.thailandmedical.news/news/sars-cov-2-triggers-mast-cell-degranulation-and-induces-respiratory-tract-epithelial-inflammation-and-injury